Unlock rheumatology coverage

Insurance said no? Appeal the decision and get covered
Evidence-backed appeals tailored to your unique situation.
Expert backed, fully customized
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
I have a long-standing history with psoriatic arthritis, rheumatoid arthritis, and plaque psoriasis that has significantly worsened over time, necessitating knee and shoulder replacements due to the extensive joint damage inflicted by my severe disease.
These conditions heavily impact my quality of life, leaving me with severe pain and significant functional limitations. My ability to work, partake in family activities, and even perform daily tasks has been compromised. This appeal is not only for medication access; it is an appeal for my well-being and a life where I can retain some degree of normalcy.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Guidance from the cited study further substantiates my case, asserting that eligibility for biologic therapy is indicated in patients with at least three inflamed joints who have failed two different conventional synthetic DMARDs for a minimum of three months each. I duly satisfy these conditions.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
The Peer-to-Peer was conducted by a physician who is NOT appropriately qualified to overrule my physician. This “plan” doctor also has not seen or examined me, is not specialized in cases such as mine and has made a different prescribing recommendation, this could be interpreted as Health Partners practicing medicine without a license.
I have copied the state insurance regulatory board as they require protection from such overreach.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
How Claimable helps you win appeals



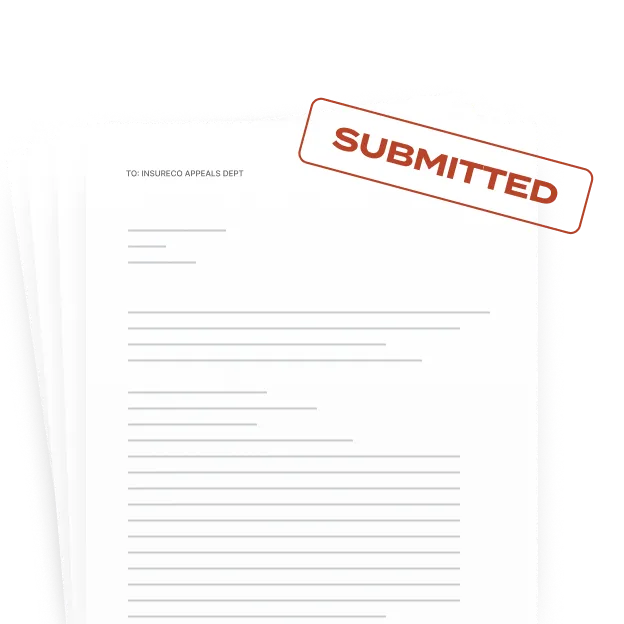

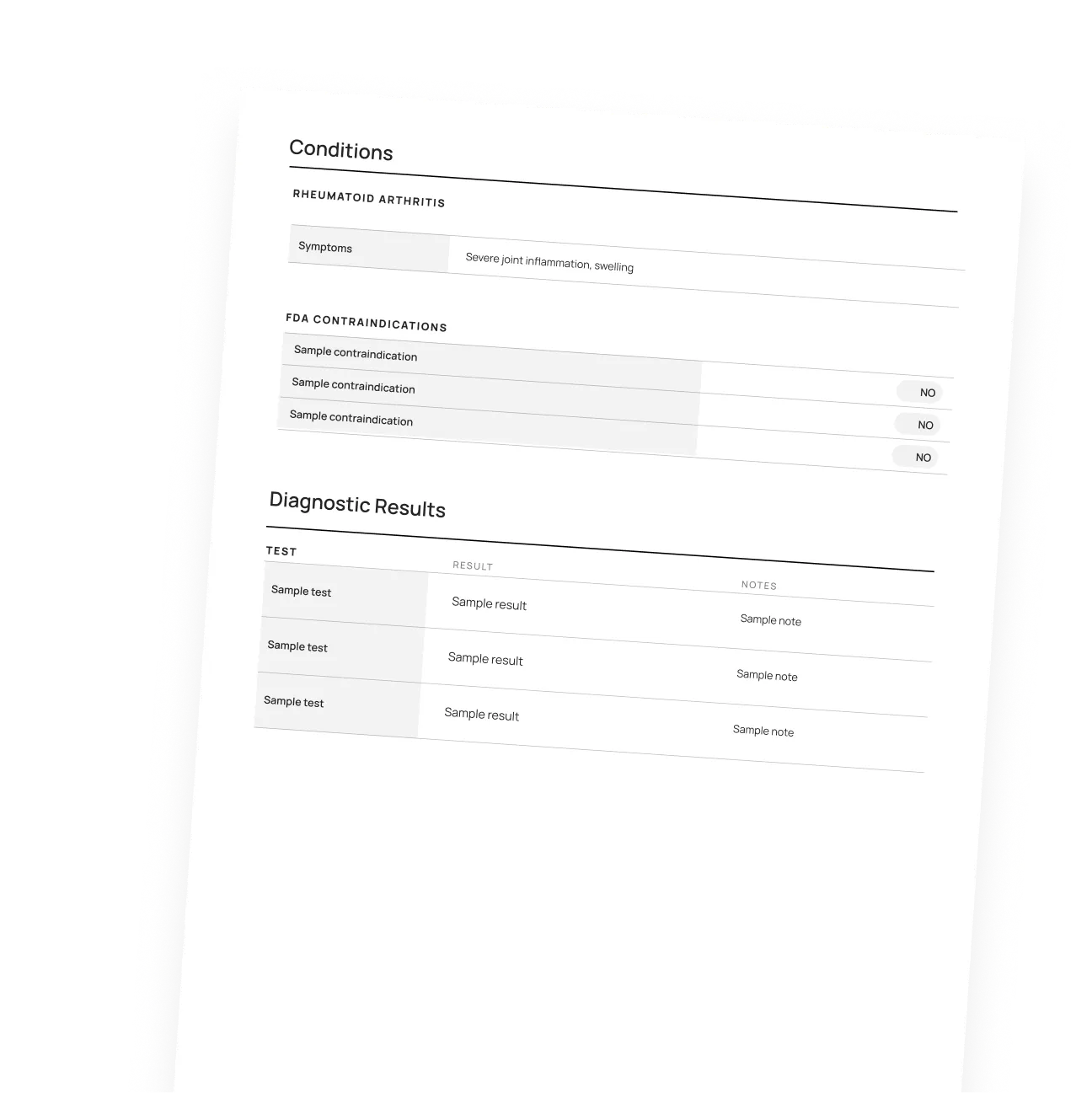
What's inside your appeal pack?

Why appeal with Claimable?
From start to send in minutes
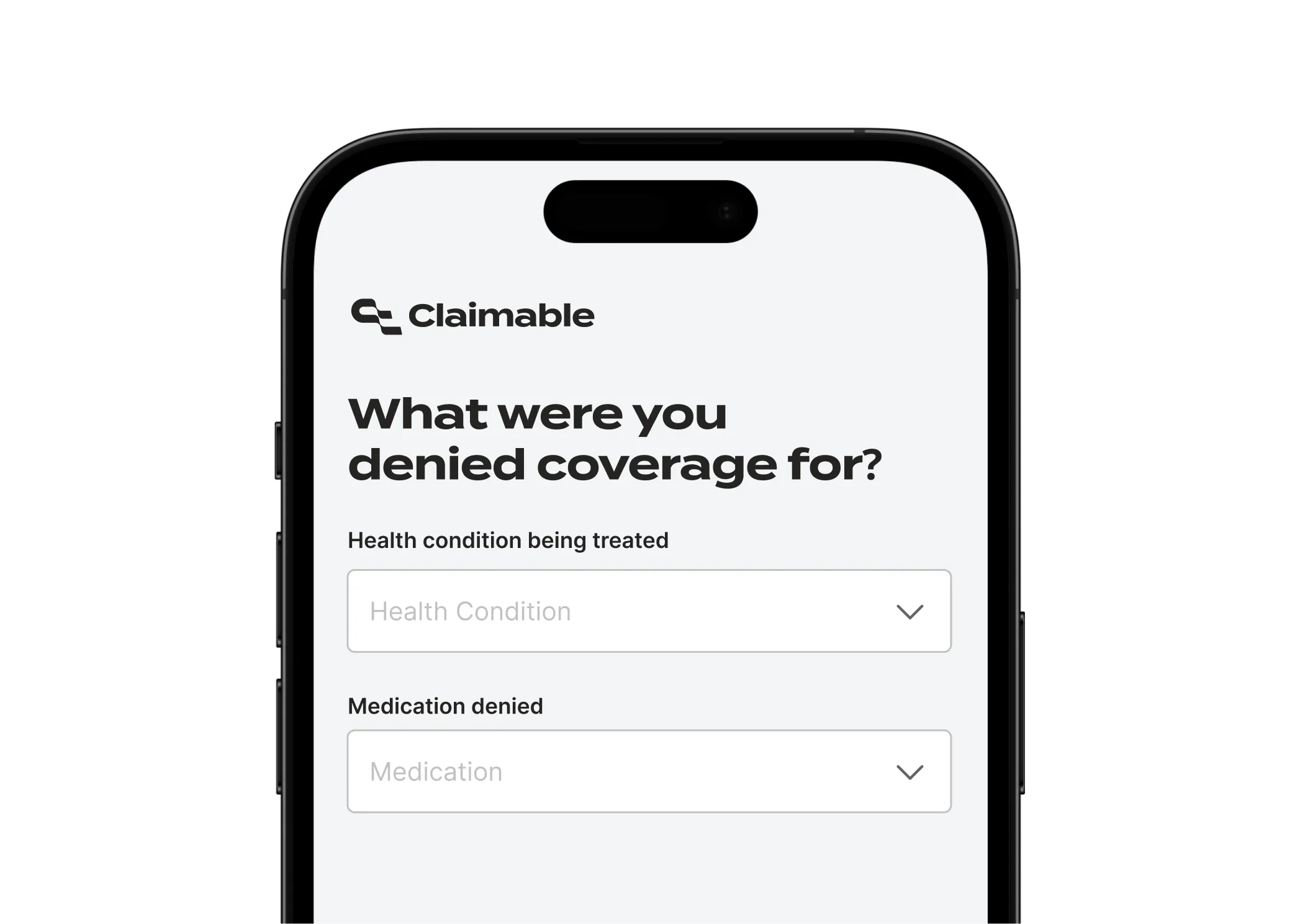
Let's get you covered.

One of our core principles is to help patients protect their rights and level the playing field with their insurance company. This includes rights to multiple appeals, fair reviews, decision rationale, exceptions when needed, and adequate network access, among others. For more, read our post on patients rights.
Claimable’s AI-powered platform analyzes millions of data points from clinical research, appeal precedents, policy details, and your personal medical story to generate a customized appeals in minutes. This personalized approach sets Claimable apart, combining proprietary and public data, advanced analysis and your unique circumstances to deliver fast, affordable, and successful results.
We currently support appeals for over 85 life-changing treatments. Denial reasons may vary from medical necessity to out of network, and we even cover special situation like appealing plans that won’t count your copay assistance towards your deductible (hint: those policies were banned at the federal level in 2023). That said, we are rapidly growing our list of supported conditions, treatments and reasons. You can quickly check eligibility and ask to be notified when your interest becomes available. It helps us know where to focus next 🙂
We think about appeal times in a few ways. First, many professional advocates and experienced patients spend 15, 30 or even 100 hours building an appeal–but with Claimable, this takes minutes. We automate the process of analyzing, researching, strategizing and wordsmithing appeals. Next, there is the process of figuring out where you will send it (hint: expand your reach beyond appeal departments), then printing, mailing and/or faxing your submission. We handle that, too. Finally, there is the time it takes to get a decision. We request urgent reviews when appropriate, and typically receive standard appeal decisions within a couple weeks.
Review periods are mandated by applicable laws, from 72 hours for urgent, 7 days for experimental, 30 days for upcoming and 60 days for received services. Our goal is to get a response as fast as possible, since most of our clients are experiencing long care delays or extreme pain and suffering.
Claims are denied for a variety of reasons, many of which blur definitions. We focus on helping people challenge denials by proving care is needed and meets clinical standards, in addition to addressing specific issues like experimental treatments, network adequacy, formulary or site of care preference exceptions. We don't support denials for administrative errors or missing information, as we think those are best handled by simply resubmitting the claim in partnership with your provider. That said, many of our most rewarding successes have been cases previously though 'unwinnable', with providers and patients who fought tirelessly for months without appropriate response or resolution.
A denial letter is a formal notice from your insurance company explaining why a claim was denied and how you can appeal the decision. Sometimes the notice is included within an Explanation of Benefits. It is a legal requirements; if you didn’t receive one, contact your insurance company.









