Dupixent coverage ending Jan 1? Do these 3 things before the deadline to stay covered
“Will not be covered starting January 1, 2026”.
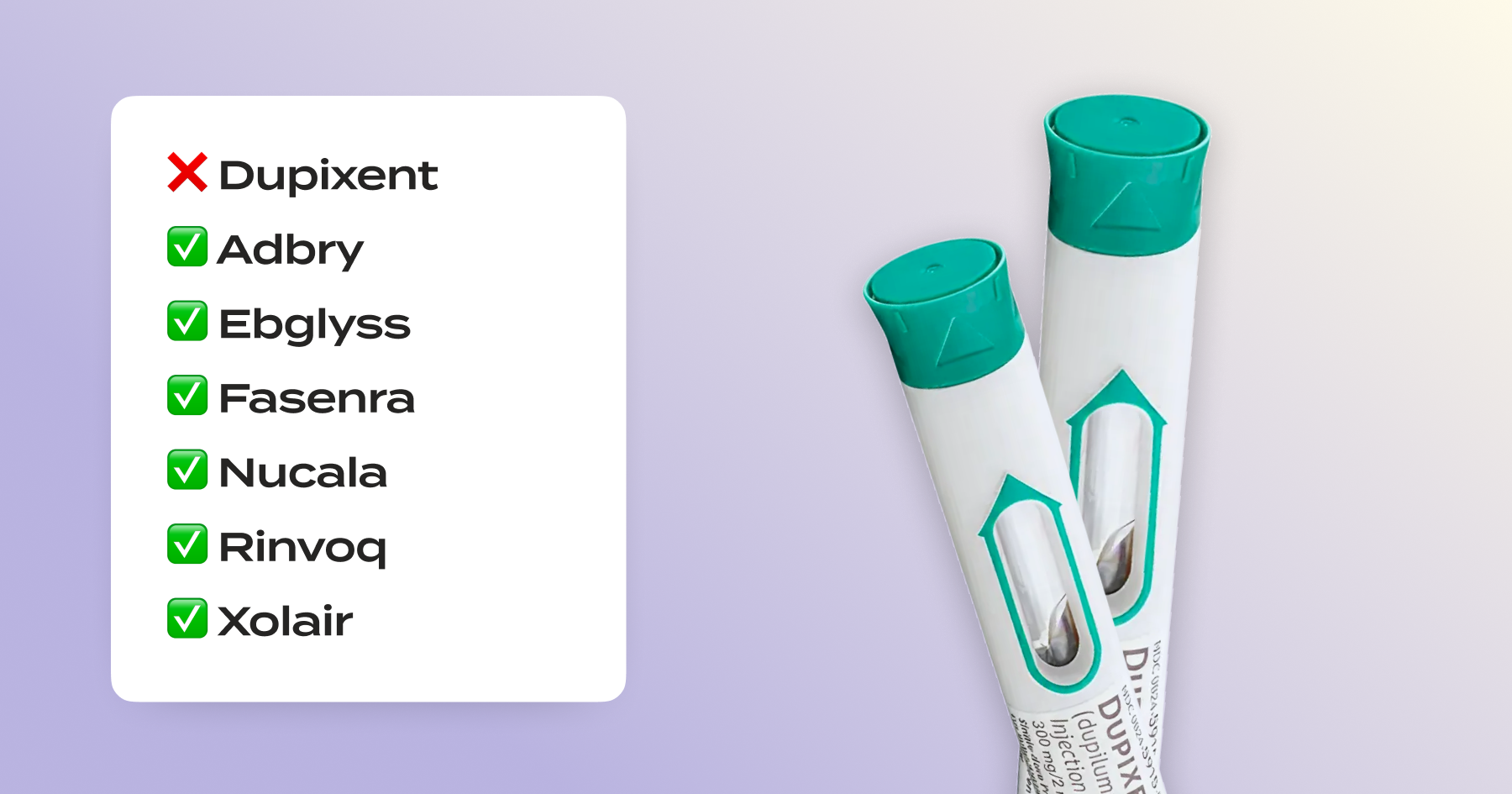
If these words look familiar, you’re not alone. In November, thousands of people began receiving formulary change letters or other coverage notices letting them know that a medication that’s working for them – Dupixent – will no longer be covered in the new year.
It can be anxiety-inducing. When you’ve found a treatment that works for you, the thought of changing can be daunting. The good news? You don’t have to. Here’s three steps to take the minute that letter hits your mailbox to keep your coverage, and stay on what works for you.
What to do now (before Dec 31)
- Ask for a 90-day refill (or “vacation override”).
Check with your pharmacy to see if you can get your last 2025 refill as a 90-day supply. This can help you stay on treatment while new coverage is reviewed. - Start your formulary exception – and label it “urgent” if you qualify.
You have a legal right to request an exception when your plan says something won’t be covered. If granted, you’ll be covered again (usually for the full plan year).
If you’re currently taking Dupixent, your request will qualify as “urgent” – meaning that your plan has to make a decision in 72 hours. In practice, we usually find this is closer to 5-7 days, but it’s still the fastest way to get coverage back. - Make a plan with your doctor to request a new approval in January
If your formulary exception is approved, you’ll be covered in the new year! But to get ahead of things, speak to your doctor now and let them know that you’re in the process of requesting the exception for Dupixent.
If your exception isn’t approved, your doctor or pharmacy will need to submit a new authorization request for Dupixent on January 1 and you can submit another exception request after that happens.
What happens on Jan 1, 2026
If you haven’t been granted an exception, here’s what you can expect in the new year with a coverage change:
- At the pharmacy: If you try to fill your prescription, the pharmacist will let you know that it’s no longer covered by your plan and see if you want to pay cash price. This can be $3000 or more without coverage, so know the sticker shock is coming and plan ahead.
- If a PA is required: Your prescriber can submit a new Prior Authorization (PA) on or after Jan 1. If the PA or exception is denied, request a pre-service reconsideration.
This is why getting ahead of the timeline matters. You can request the formulary exception the minute the coverage notification letter hits your mailbox – so you can confirm new year coverage before January 1 and skip the pharmacy headaches and PA complexity.  
A realistic timeline to stay covered
Start now
- Request a 90-day supply of your medication.
- Get your formulary exception request submitted (use our step by step guide here, or get started fast by using Claimable)
If your first exception request is denied
- Request a reconsideration of the request. When you make this second request, it’s required to be reviewed by a qualified clinician.
- If you still disagree, you can escalate to have your request reviewed independently by the Office of Personnel & Budget Management. 
On January 1 (if you still don’t have coverage)
- Have your doctor submit a new Prior Authorization for Dupixent.
- If that gets denied, file a new formulary exception request.
Any time after your request has been submitted
- Request your claim file and relevant plan documents – you have a federal right to obtain all the documents they’ve used in making decisions about your request, and you can use this to strengthen your case. 
Need help with the process?
Use our Dupixent appeal tool for the fastest, easiest way to get your exception request drafted and filed. Fast, easy, and free for eligible patients.
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!