Dupixent not covered by FEP Blue for 2026: What your letter means and how to keep coverage.
In early November, many FEP Blue members opened a letter saying Dupixent won’t be covered next year. The options? Switch to an alternative medication, or pay full price.
At Claimable, we help people fight insurance denials every day. Forced switches like this one are all too common in our world, and that means we know exactly what to do when they happen.
Let’s break down these switch letters, what to do if you got one, and how to use Claimable to file your formulary exception so you don’t have to switch. Already have the letter? Sign up here to be notified the minute you can start filing your appeal with Claimable – coming late November
Quick Summary: What you need to know
- Coverage is changing for Dupixent on some FEP Blue formularies in 2026.
- You can ask the plan to keep covering Dupixent by filing an appeal to request a formulary exception.
- If you’re currently taking Dupixent, your appeal qualifies for expedited review – plans should issue a decision within 72 hours upon receipt.
- It’s possible to get a 90-day refill after three 30-day fills, which could help you prevent care gaps by contacting the CVS Specialty Pharmacy Program at 1-888-346-3731.
- If the initial appeal is denied, FEHB members can seek an external review by OPM. 
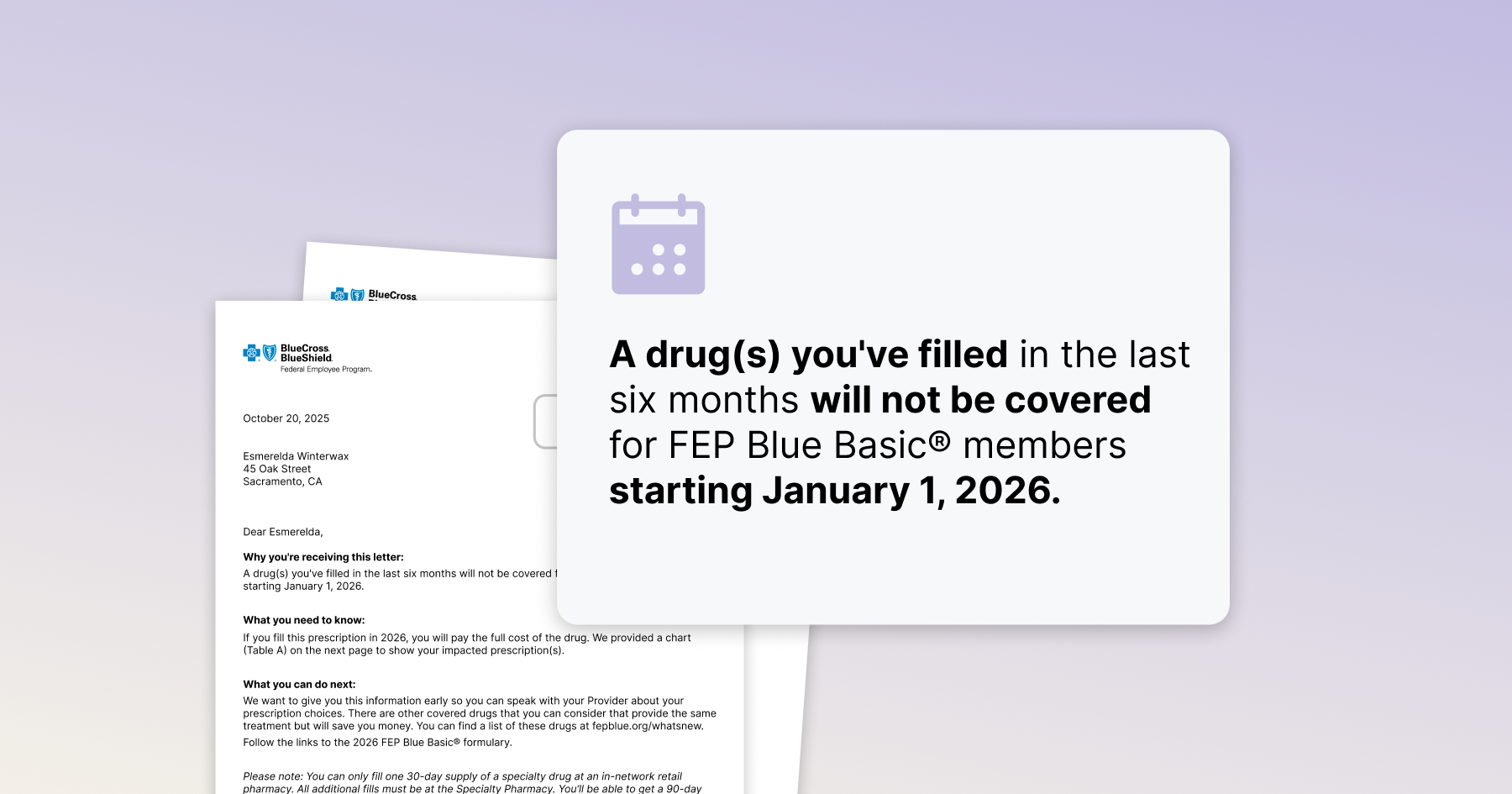
What your letter says—translated
The notice you received follows a predictable pattern. Here’s each section, decoded.
"A drug you’ve filled will not be covered for FEP Blue members starting January 1, 2026."
What it means: This is the formulary change; Dupixent is no longer covered. Unless you take action, claims for Dupixent will not be approved on Jan 1.
What to do now: Begin your formulary exception appeal so coverage is in place before the new year.
"If you fill this prescription in 2026, you will pay the full cost of the drug."
What it means: Your pharmacy will charge you cash price at the counter unless an exception is approved. For Dupixent, this can be in the thousands of dollars per fill.
What to do now: Upload your letter when you start your Claimable appeal; if your initial appeal is denied, we’ll continue to escalate your appeal all the way through plan reconsideration and final OPM review to make sure you don’t get stuck with sticker shock at the counter.
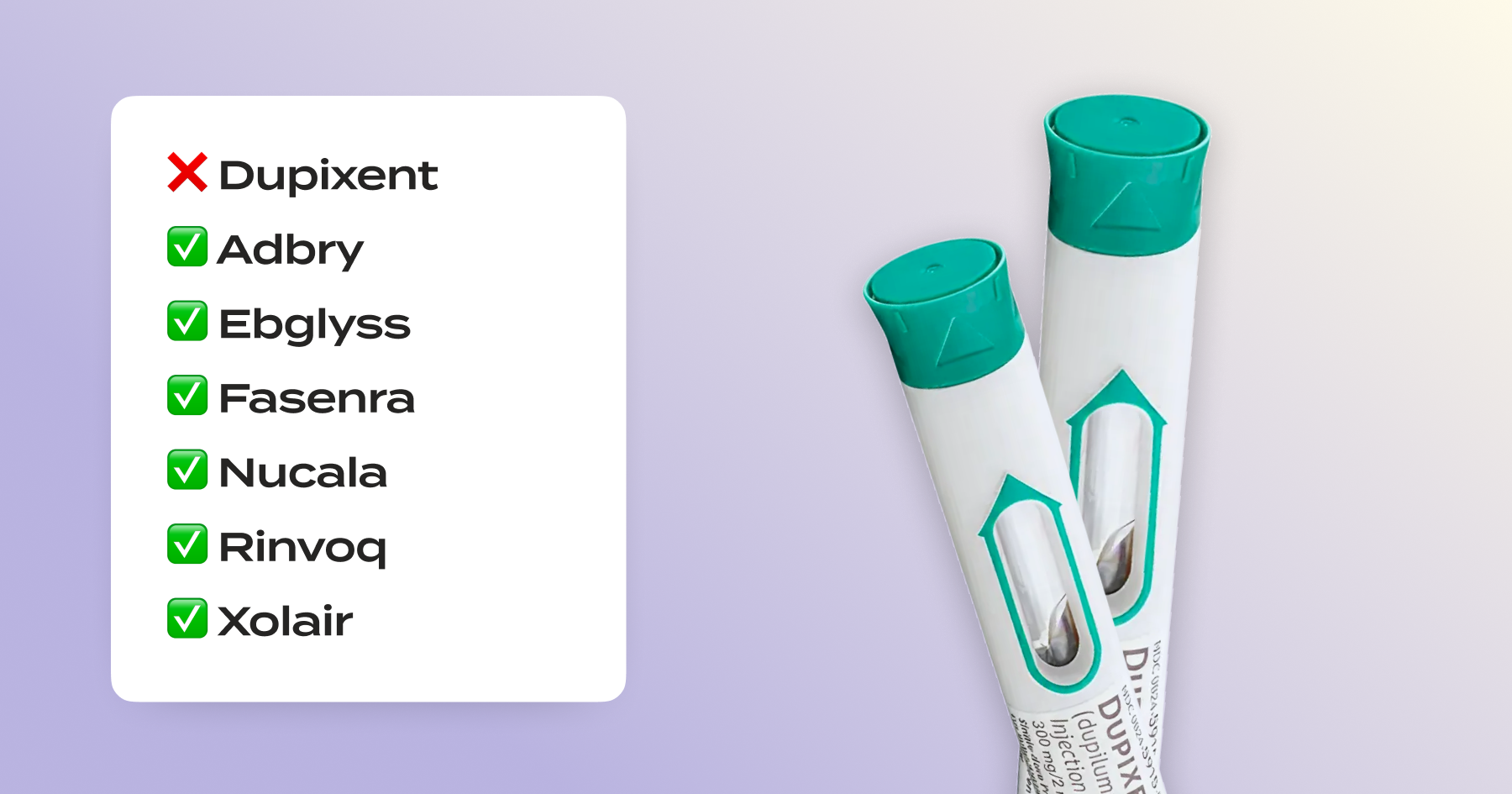
"Speak with your Provider about your prescription choices / there are other covered drugs that you can consider."
What it means: They're suggesting alternatives like Adbry, Ebglyss, Fasenra, Nucala, Rinvoq, and Xolair—but you don't have to switch if alternatives are less effective, tolerable or are unsafe. For some conditions (EoE, prurigo nodularis, bullous pemphigoid), Dupixent is the only FDA-approved treatment—these alternatives aren't even approved for your condition.
What to do now: Talk to your doctor about getting medical records that show you’ve tried and failed alternatives and/or a letter of medical necessity that supports why Dupixent is right for you.
Specialty Pharmacy Program details
What it means: Generally, this shouldn’t be a change – it’s just a reminder of how pharmacy dispensing works under your plan.
What to do now: If you’re eligible for a 90-day fill, put in a request for one now. That way, you’ll have a backup plan if there’s any gaps or delays in getting coverage.
"Provider can submit a formulary exception at fepblue.org/claim-forms."
What it means: What they don't tell you is that you can file yourself. FEP's policy explicitly allows "members to apply for coverage of a non-covered drug." You don't have to wait for your provider. Claimable ensures your exception includes all the clinical evidence, policy requirements, and legal protections for the strongest case.
What to do now: Get ready to appeal by signing up for notifications the minute they launch—expected 11/27/25. 
Your rights (and why timing matters)
Federal rules require plans to offer a way to request access to clinically appropriate non-formulary drugs. When you’re on current treatment or a delay could harm you, the plan should process an expedited exception and issue a decision within 72 hours of receiving it, with most patients notified within 5-7 days of the decision.
FEP also has a unique safety net: after the plan’s reconsideration, you can ask OPM (the federal agency that oversees FEHB) to review the case. 
Why is FEP Blue suddenly denying Dupixent?
Plans update their formularies – lists of drugs covered on their plan – every year. When a drug comes off that list, coverage stops unless you switch to a covered option or get an exception approved.
Formulary changes are largely cost control measures for insurers, and they can happen when they deem a medication to be too expensive or, in the case of the recent CVS Caremark Zepbound to Wegovy formulary change, receive a rebate from a rival manufacturer.
This is called non-medical switching—forcing patients to change medications for financial reasons, not medical ones. While many states have laws restricting this practice, federal employee plans like FEP Blue aren't bound by state insurance laws, and Congress hasn't passed federal protections yet.
But you still have rights. Federal regulations require plans to offer a formulary exception process when switching would be clinically inappropriate. Your appeal invokes that right—demonstrating that Dupixent is medically necessary and that the suggested alternatives won't work for you.
Two things to do today:
- Start your appeal. With Claimable, you can draft and submit your request in minutes (free for qualifying Dupixent patients).
- Request medical records. Ask your doctor for documentation showing failed alternatives and why Dupixent is medically necessary.
Understanding your options: Will I be forced to switch to something else?
Not automatically. The key is demonstrating why the alternatives won't work for you—and that forcing you to switch would be clinically inappropriate.
Here's how to build a strong case:
- Explain why you can't take alternatives:
- You've already tried and failed similar treatments (document drugs, dates, outcomes)
- Alternatives were never effective, or lost effectiveness over time (therapeutic failure)
- You experienced negative or harmful side effects with alternatives (adverse events)
- Alternatives are contraindicated with another medication or condition, have an applicable FDA warning, or otherwise pose clinical risks for you
- Switching could cause disease flares or setbacks
- Showcase where Dupixent is uniquely appropriate
- For EoE, prurigo nodularis, or bullous pemphigoid: Dupixent is the only FDA-approved treatment—the suggested alternatives (Adbry, Ebglyss, Fasenra, Nucala, Rinvoq, Xolair) aren't even approved for these conditions
- For other conditions: Age restrictions, disease phenotype, or lack of on-label alternatives may make Dupixent the only appropriate option
When supported by strong clinical evidence and proper documentation (like in a Claimable appeal), you have a strong chance of winning your exception.
How to file an FEP Blue formulary exception for Dupixent
1) Gather the essentials (10–15 minutes)
- Your coverage change letter (the one saying Dupixent won’t be covered in 2026)
- Plan details (Basic/Standard/Focus, member ID)
- Treatment history: drugs tried/failed, bad side effects, contraindications, ER visits
- Medical records or letter of medical necessity from your doctor (if available)
2) Draft your exception request.
Write a formal letter that includes:
- Your diagnosis and treatment history
- Why Dupixent works for you and alternatives don't
- Clinical evidence supporting medical necessity
- Policy/legal citations backing your rights to continued coverage
Seem daunting? Claimable drafts a comprehensive formulary exception request—including all clinical and policy evidence—from a short survey. Free for qualifying Dupixent patients with commercial insurance.
3) Submit your exception appeal
- DIY route: Follow the process detailed on pages 138-142 of the 2026 Standard and Basic Plan Brochure
- Easier path: File directly through Claimable in just a few clicks. No uploads, downloads, or post office visits.
4) Request expedited review if you're currently on Dupixent
If you're currently taking Dupixent or a delay could harm you, federal law requires expedited review with a decision within 24-72 hours (though realistically it takes 5-7 business days). Claimable automatically flags this when you qualify.
5) If your initial request is denied
You can request plan reconsideration, and FEHB members can escalate to final administrative review by OPM under the disputed claims process. Claimable guides you through each escalation step—we keep fighting until you win.
6) If approved but your copay is still too high
You may be eligible for Dupixent's copay assistance program, subject to program rules and federal restrictions. Contact Dupixent directly or ask your pharmacy about eligibility and enrollment: https://www.dupixent.com/support-savings/copay-card
Get started now
How Claimable helps (free for qualifying Dupixent patients!)
Claimable appeals succeed in over 80% of cases. Here's how we help:
- Custom appeal: We build a fully personalized, expert-backed formulary exception request for your unique situation
- Complete filing: We instantly submit it via fax and mail with all required documents, clinical evidence, and policy citations your plan needs
- Expedited review: We request fast-track decisions when you qualify and monitor deadlines
- Full escalation: If denied, we guide you through reconsideration and OPM review—we keep fighting with you.
Free for Dupixent patients with commercial insurance (including FEP Blue) through our partnership with Dupixent's patient support program.
Sources & helpful links
- Prior Authorization Form and Dupixent FEP Criteria
- Medical Exception Form for FEP Blue Focus, Basic and Standard
- 2026 Formulary for FEP Blue Focus, Basic and Standard
- 2026 Plan Brochure for FEHB FEP Blue Focus, Basic and Standard
- 2026 Plan Brochure for PSHB FEP Blue Focus, Basic and Standard
- Your right to an exception and expedited decisions (45 CFR 156.122(c))
- Specialty Pharmacy Program details and contact info
- FEHB/OPM review (FEHB Handbook and program materials)
- Authorized Representative Designation Form
The bottom line – you don't have to switch from Dupixent
A coverage change letter isn't the end of the road—80% of Claimable appeals succeed.
Formulary changes harm patients who've spent years finding stable, effective treatment. You don't have to accept this. Challenge the decision, get your doctor's support, and file your exception.
Claimable builds and files your Dupixent exception for free* for qualifying patients. But that’s not your only choice. If you’re one of the thousands of people who got the Dupixent letter, take a breath. What’s happening here is called a formulary change, and you can challenge it – and win. Many people in scenarios like this one will be able to keep coverage by filing something called a formulary exception.
*Free for Dupixent patients with commercial insurance (including FEP Blue) through our partnership with Dupixent's patient support program.
Get started now
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!