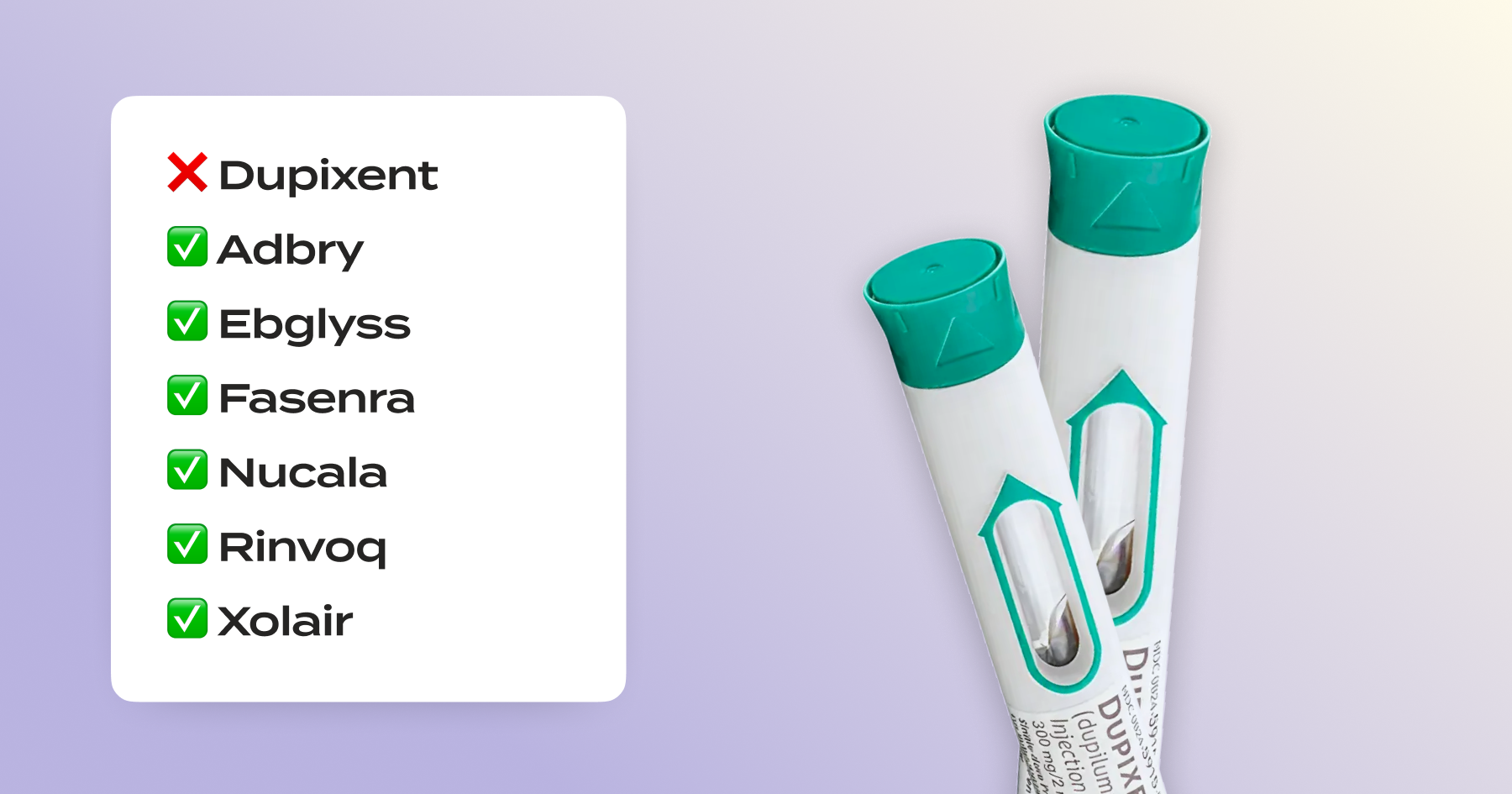
FEP Blue denied Dupixent for 2026? Your legal rights and how to stay covered.
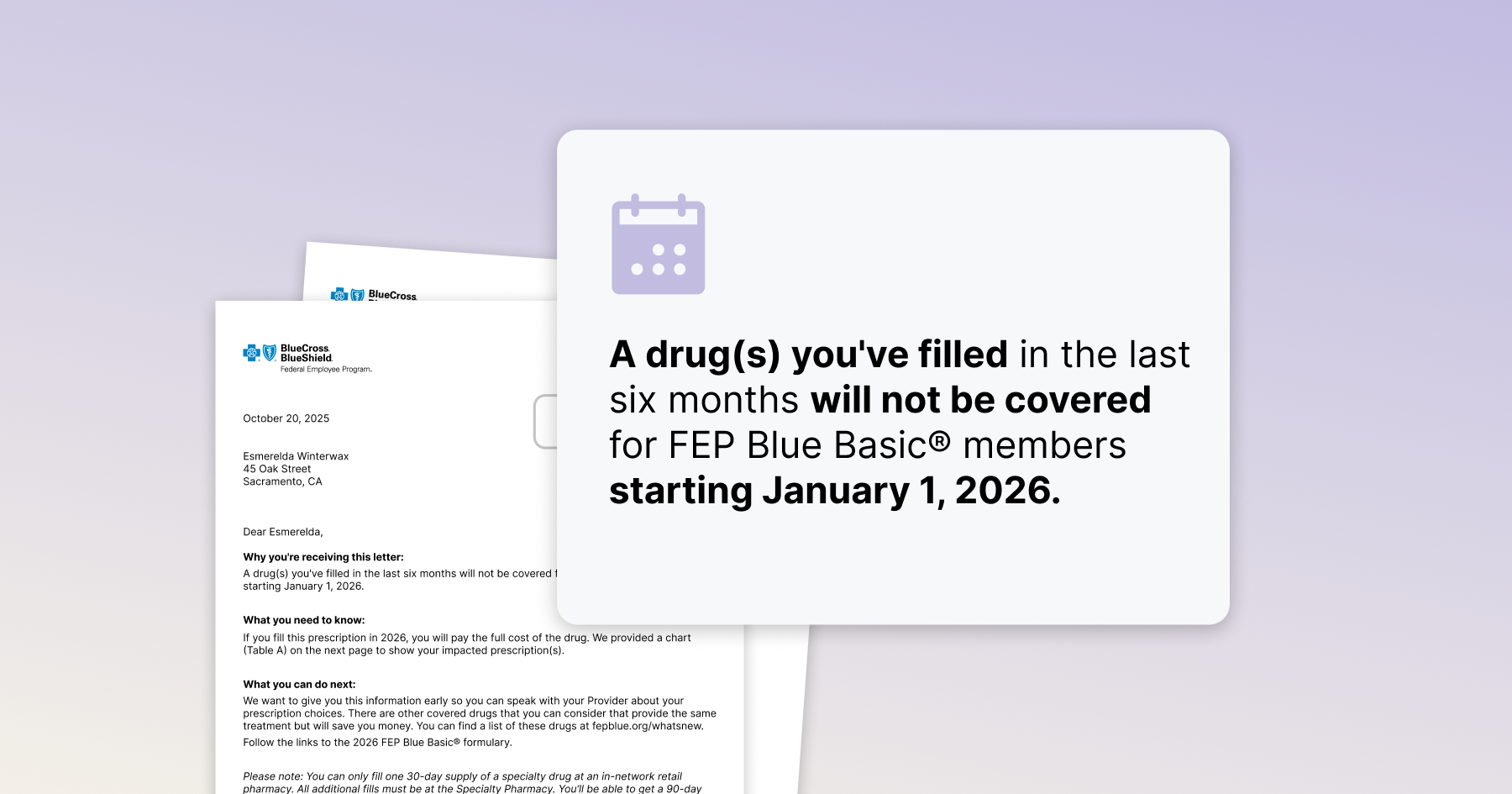
If you’re currently taking Dupixent and got a 2026 “not covered” notice, you might be wondering – do I have to switch medications and start all over again?
The short answer: No. Many people don’t know this, but when insurance denies your meds or asks you to change to something else, you don’t have to just accept a switch. Under federal law as well as FEP Blue’s own policies, you have rights that protect you and can help you get coverage back for the medication that’s working for you.
BCBS Formulary Exception Process
The Formulary Exception process allows members to apply for coverage of a non-covered drug if they have tried and failed the covered drug(s). If the exception is approved, the non-covered drug will be covered.
Let’s break down your essential rights – and how to use them to stay covered.
Your rights overview – what you can ask for:
- Right to request a formulary exception. You (not just your doctor) may ask the plan to cover a non-formulary drug (one that isn’t on their “covered list”) when it’s clinically appropriate. If the exception is granted, typically coverage must be provided to the end of the plan year (not just a one-time fill).
- Right to an expedited decision if you’re mid-treatment. If you are already taking the medication or if delay poses a risk of serious harm, the plan must issue an expedited decision on your formulary-exception request within 72 hours when you are undergoing a current course of treatment using a non-formulary drug.
- Right to clear notices and to access your file. FEP denial notices must identify what was denied and why, and must provide any policies or criteria used upon request. You are also entitled to review and obtain copies of all materials the plan relied on. We strongly recommend requesting your claim file with every denial to verify the plan’s rationale and proper handling.
- Right to reasonable reconsideration timelines. For non-urgent pre-service disputes when you are not already on treatment, you have 6 months to request reconsideration. The plan then generally has 30 days to respond unless you request an urgent/expedited review.
- Right to a qualified reviewer. For appeals, FEP must consult a clinician with appropriate training and expertise who was not involved in the initial decision to assess the medical necessity of your treatment.
- Right to escalate to OPM (final FEHB review). If the appeal is denied—or the plan does not follow required claims procedures—you may take your case to the U.S. Office of Personnel Management for final administrative review. Expedited formulary-exception requests are typically resolved within 72 hours and may be submitted at the same time as your internal review. Standard OPM reviews generally take 30 days.
How to use these rights to get covered
The important stuff. Lean on your rights as a member of the plan to hold your insurer accountable – you deserve timely responses, fair determinations, and appropriate coverage. Here’s how to make it happen.
1) Ask for a formulary exception
Tell the Plan you’re appealing the non-coverage notice and requesting a member reconsideration/formulary exception for Dupixent based on medical necessity.
If you’re currently on Dupixent (or delay could seriously harm you), mark it Urgent—pre-service to trigger the expedited review timeline.
Follow our step-by-step guide for exactly how to do this – or use Claimable to make it easy.
2) If they reject your exception request, ask for your claim file
You’re entitled to a review that considers everything you submit and – when medical judgment is involved – uses a clinician with relevant expertise who wasn’t part of the original decision. You can also review and copy all relevant materials at no charge.
3) Escalate to OPM for a final decision
For non-urgent pre-service issues, you have 6 months to request reconsideration; the Plan must decide within 30 days (with defined clocks if it asks you for more info). Urgent pre-service reconsiderations, including for any are due in 72 hours. If the Plan upholds the denial—or doesn’t follow required processes—you may appeal to OPM. For urgent pre-service claims, you can request simultaneous OPM review.
What counts as a strong basis to keep Dupixent?
Federal rule §156.122(c) says plans must have a way to get an exception to access clinically appropriate non-formulary drugs; “exigent circumstances” include being in a current course of treatment.
If you have previously tried alternatives that were failed, were intolerable, are contraindicated, are off-label for your diagnosis/age, or carry unacceptable risks versus your stable response on Dupixent, that’s a compelling medical necessity to document.
Your notices must be understandable and specific FEP notices (EOBs and adverse determination letters) must identify the claim, list key details (date of service, provider, amount), and inform you that diagnosis/procedure codes are available on request. Use this to pinpoint exactly what the plan relied on – and what evidence to add.
It sounds a bit complicated – because, frankly, it is. There’s a lot of insurance, legal, and clinical complexity to wade through to get it right. That’s why we’re here.
How to appeal easily and effectively
Use Claimable. Our free service for Dupixent will draft your appeal, source the exact regulations and provisions, compile clinical evidence tailored to your condition, and file by fax/mail for you – plus handle your OPM escalation if needed.
If you still want to DIY it – or just understand the nuts-and-bolts steps – dig into our step-by-step FEP Blue appeal guide for Dupixent here.
Sources
- Formulary exception & expedited decision (24h/72h) — 45 C.F.R. § 156.122(c): standard & expedited exception processes, decision deadlines, and duration of coverage.
- FEP Blue Standard/Basic 2026 Brochure (official plan rights & timelines) — pre-service decision/reconsideration timelines; simultaneous OPM review for urgent claims; notice and file-access rights; disputed claims process.
Use your rights - and get covered
You have the right to ask for Dupixent to stay covered now, to get a fast answer if you’re mid-treatment, to a qualified, fair review on a clear timetable, and to a final OPM review if needed. Use those rights so you don’t have to start 2026 on the wrong medicine. We’re here to help make it happen.
Start your appeal now
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!