How to get a formulary exception approved for Dupixent: A step by step guide to appealing an FEP Blue denial
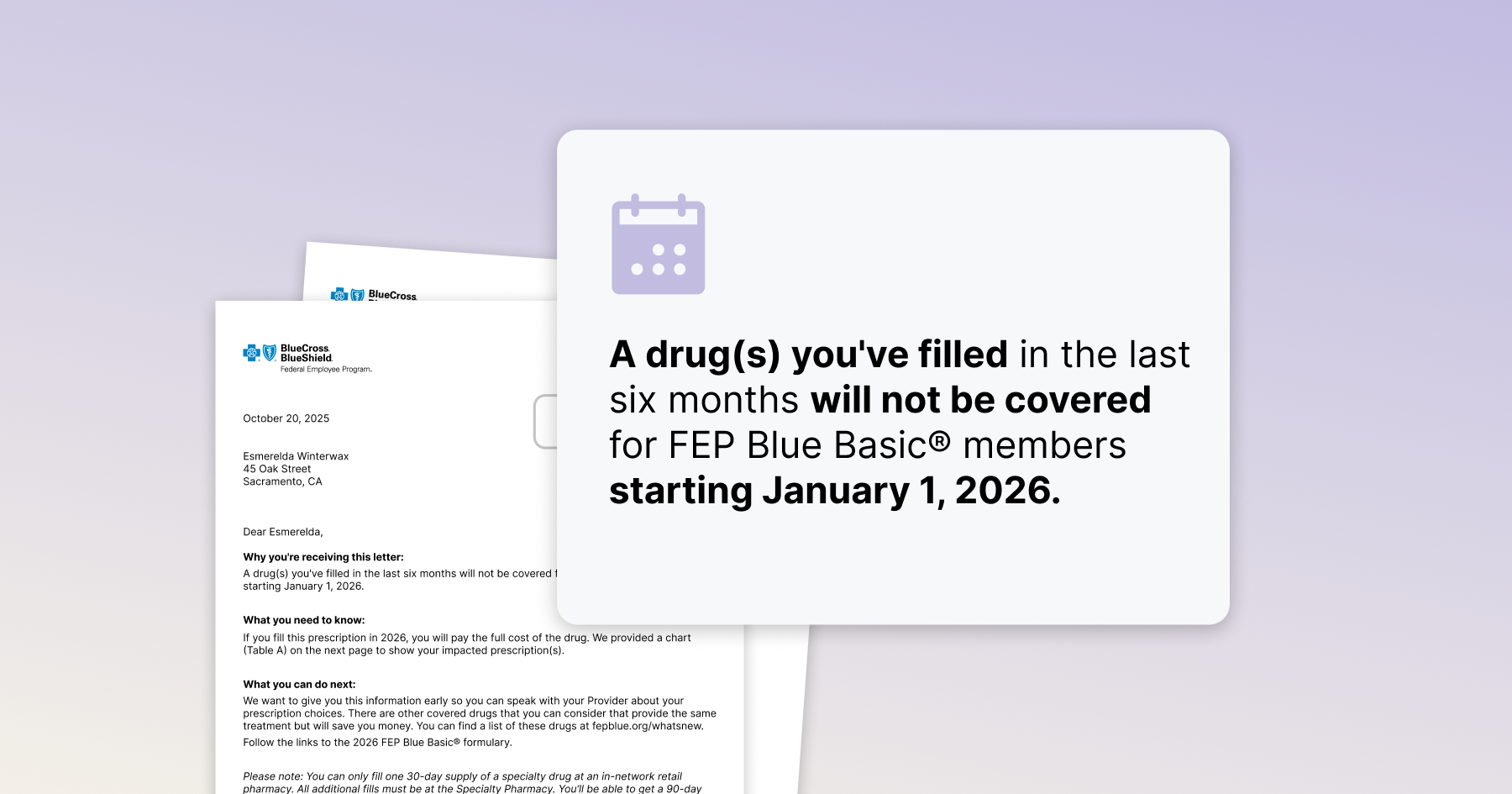
If you're on Dupixent and got a notice saying it won't be covered in 2026, don't settle for switching. Under FEP Blue, you can appeal the coverage decision as a member and request a formulary exception to keep Dupixent covered when it's medically necessary.
But filing an appeal isn't always easy or obvious – in fact, the process is often buried in PDFs and plan documents. Let's make it easy: Follow our step-by-step guide for exactly what you need to do to appeal and request a formulary exception – and get it approved.
Choose your path: You can take the DIY route to appeal yourself, or use the fully-guided Claimable experience (free for qualifying Dupixent patients with commercial insurance, including FEP Blue). We'll draft your appeal letter requesting a formulary exception, source all the right evidence, and mail and fax it all with just a few minutes of your time.
Note: Your doctor can also file a medical exception form on your behalf, but many providers face time constraints. We recommend filing a member appeal yourself to ensure it gets done quickly.
Quick summary:
- Appeal timing: If you got the notice letter, don't wait until the coverage change kicks in on January 1. You have up to 6 months to file your appeal, but we recommend filing now to avoid coverage gaps.
- Where to send: Mail your appeal to Service Benefit Plan, P.O. Box 52080, Phoenix, AZ 85072-2080 or fax to 1-877-378-4727
- Urgent cases: If you're already taking Dupixent, mark your appeal "Urgent—pre-service." FEP must issue a decision within 72 hours (realistically 5-7 business days).
- What to send: Follow our member appeal guide below to request a formulary exception. (Your doctor can also file a medical exception form, but we recommend filing a member appeal to ensure timely action.)
- Escalation options: If your appeal is denied, you can request reconsideration, then escalate to OPM for final administrative review.
Step 1 — Prepare (documents, addresses, and your case theory)
Gather documents:
- Your coverage notice and any denial letters received when trying to refill.
- Your insurance card and and member ID.
- Relevant medical records: therapies tried, dates/durations, outcomes (failure, intolerance), and any contraindications.
Decide urgency: If you’re in a current course of treatment or delay could seriously jeopardize health/function, you can file as Expedited (72 hour mandate, 5-7 day reality).
Sketch your case: Note why Dupixent is appropriate for your diagnosis and why the listed alternatives are not (failures, intolerance, phenotype/label mismatch, age limits). Take a moment to reflect: How Dupixent has helped you, and what your experience was on other treatments. Personal impact and details about symptoms and benefits are key for a strong appeal/
Need help? Check out our alternatives breakdown and condition-specific blog posts for a deeper dive.
Step 2 (Optional) — Ask your doctor to write a Letter of Medical Necessity (LOMN)
Your doctor writes the LOMN; you submit it with your appeal. Ask for a short, specific letter that includes:
- Diagnosis & severity (objective measures where applicable).
- Prior therapies (names/dates/doses) and outcomes (failure, intolerance, etc.).
- Contraindications/risks with covered alternatives
- Why Dupixent is appropriate for you now (phenotype fit, stability, clinical goals).
- Risk of switching or treatment interruption (flares, ER visits, disease regression, etc).
- Current response if you’re already on Dupixent (what’s improved, what’s prevented).
Shoot them a message in your portal to make the ask – try our sample message below for a quick and effective request. Tip: Make it as easy as possible for your provider with Dupixent’s template – just drop the link into a message to them in your prescriber portal.
Hi Dr. [Name],
I received a notice that Dupixent won’t be covered in 2026. I’m filing a member reconsideration / formulary exception request and need a brief Letter of Medical Necessity on your letterhead.
Could you please include:
- Diagnosis & severity (scores/tests if used)
- Prior therapies with dates and outcomes (failure/intolerance/contraindication)
- Why Dupixent is appropriate for me now
- Risks of switching/interrupting treatment (health risks, function loss)
- If I qualify for an urgent review (current treatment, serious disease)
- Current response on Dupixent (if applicable)
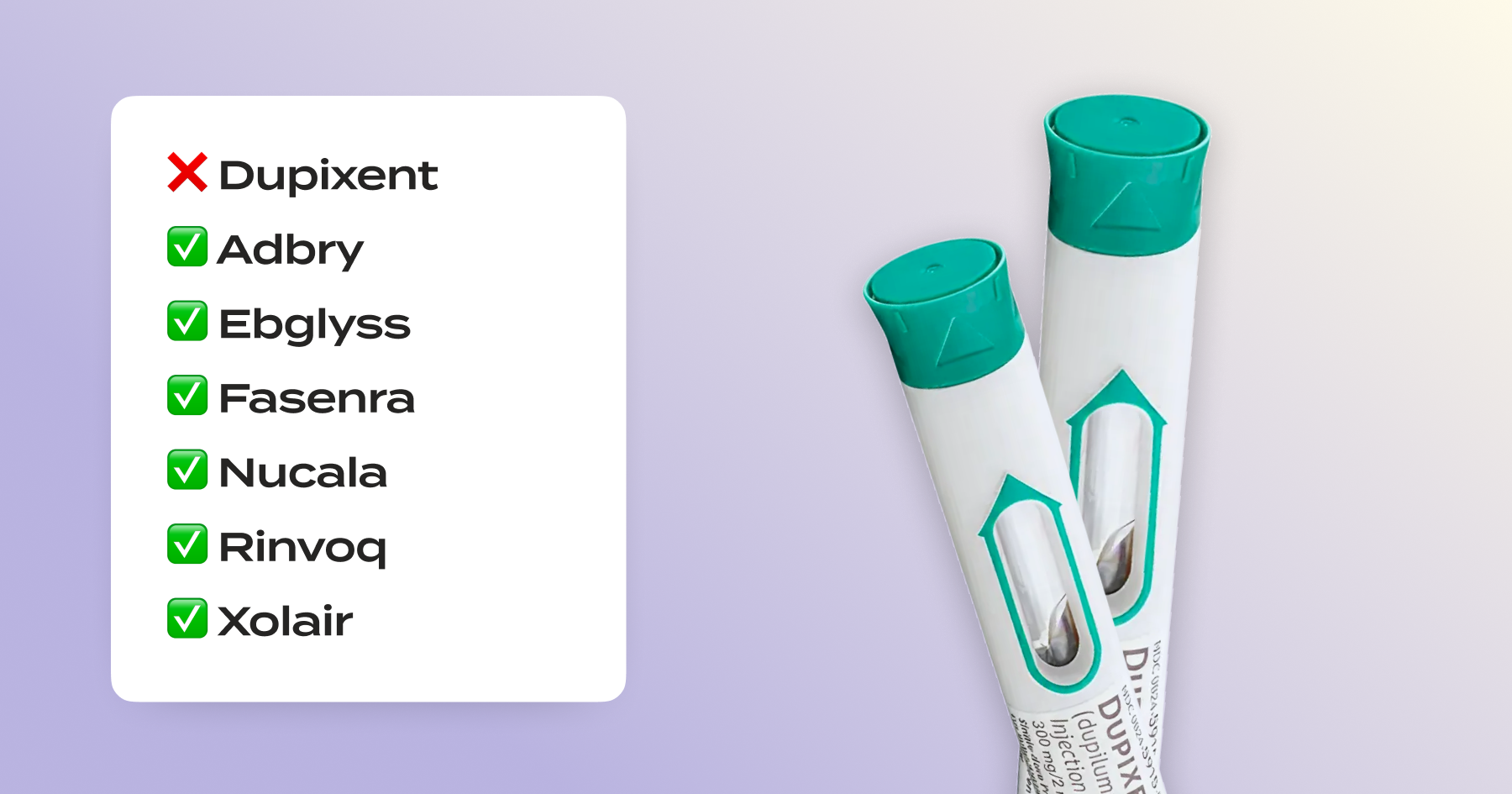
Of note, FEP Blue is suggesting I use one of these covered alternatives—so providing specific details about these medications is important: Adbry, Ebglyss, Fasenra, Nucala, Rinvoq, and Xolair. For reference, you can also review the Prior Authorization Form, Dupixent FEP Criteria and Medical Exception Form.
Here’s a Dupixent-specific template you can use. If possible, please upload the letter and any relevant chart notes or history so I can attach it to my appeal.
Template link: https://www.dupixenthcp.com/dam/jcr:9c7e414d-99b5-40a1-acd0-b77173536029/US.DUP.25.04.0698-DMW%20AD%20Sample%20Appeal%20Letter-%20Letter%20of%20Medical%20Necessity.doc
Thank you so much!
Step 3 — Build your request
Write your formulary exception request letter. Include:
Subject: Member Appeal Requesting Expedited Reconsideration of Adverse Benefit Determination — Dupixent Non-Coverage (effective 1/1/2026)
Opening: You’re appealing the plan’s non-coverage notice and requesting continued coverage based on medical necessity. It’s urgent becasue you are at risk of a gap in treatment, so add “Urgent—pre-service.”
Details to include: Your diagnosis and documentation; response on Dupixent; prior therapies + outcomes; clinical evidence supporting medical necessity; why listed alternatives are not appropriate for you; policy and legal precedent if you have it.
Attach: LOMN, key chart notes, the coverage notice.
Submit your packet as soon as possible (must be within 6 months) – to the address shown on your EOB/plan materials for pharmacy claims (Retail/Mail Service/Specialty Drug Program). Keep a copy and proof of delivery.
How to put it together:
- The DIY route: Assemble your appeal letter and supporting documents into a single PDF document. Include a 1-page summary on top.
- The guided option (Claimable): You fill out a short survey to provide all the relevant info; we draft the letter, cite all the evidence, mail and fax for you (free!).
Step 4 — Know the timelines (so you can escalate on time)
- If you’re currently taking Dupixent: This qualifies as urgent and the plan must decide within 72 hours of receiving your exception request (though in practice many take 5-7 days to notify you of decision).
- Otherwise: For non-urgent appeals, the plan decides within 30 days of receiving your reconsideration (if it asks for more info, you have 60 days to supply it; then the plan decides within 30 days of when that info was due/received).
If you disagree with the plan’s reconsideration – or it doesn’t decide on time – go to Step 5.
Step 5 — Escalate to OPM (the final FEHB review)
If the plan upholds the denial (or misses its deadline), you can request a final administrative review by OPM. Deadlines are strict (e.g., 90 days after the Plan’s reconsideration denial; 120 days if the Plan failed to respond on time). Your OPM packet should include your statement of why the Plan is wrong, supporting medical documentation, and copies of all correspondence.
- The DIY route: If your first request is denied and you want to escalate to OPM on your own, you’ll re-submit your appeal and all its documentation along with a statement supporting why you believe the initial decision was wrong.
When you’re ready, send it to U.S. Office of Personnel Management, Healthcare & Insurance, Federal Employees Insurance Operations, FEHB 1, 1900 E Street NW, Room 3425, Washington, DC 20415-3610. Find more details and instructions on page 141 of the 2026 FEHB FEP Standard and Basic Plan Brochure. - The guided option (Claimable): Once you tell us that your first request was denied, we automatically initiate the OPM review process – updating your statement and documents, clearing it by you for review, and putting it in the mail.
FAQs
Who should file my appeal—me or my doctor?
Either you, your designee, or your doctor can file. Even the most dedicated providers face limits on how much time they can spend fighting denials. Claimable ensures your exception includes all the clinical evidence, policy requirements, and legal protections that give your case the strongest chance of success—details that often get missed when providers are overwhelmed. If needed, your insurer can contact your provider directly to submit additional forms and documents.
How long does the appeal process take?
It depends on the type of appeal — but the sooner you file, the sooner you’ll hear back. Insurers often exceed legal deadlines. Claimable ensures your appeal is filed quickly and that mandated timelines are clearly documented, so any delay is on them, not you.
- Formulary exception appeals: Must decide within 72 hours if a delay affects current treatment or could harm your health. Reality: Often takes 5–7 business days.
- Prior authorization appeals: Must decide within X days (expedited) or 7–15 days (standard). Reality: Usually 1–2 weeks, unless actively escalated.
- Post-service appeals (after a claim is denied): Must decide within 30 days for internal review, 45+ days for external review. Reality: Commonly 6–10 weeks, sometimes longer.
What if I already switched?
You can still appeal to restore coverage for Dupixent – ensure your doctor documents if switching caused negative or harmful symptoms or is unsafe/inappropriate for you, and include this information in your appeal.
How long do I have to appeal an FEP Blue denial?
The appeal window is 6 months after the initial denial.
What counts as an urgent pre-service appeal?
Under 45 CFR § 156.122(c)(2), you have the right to request an expedited formulary exception review when exigent circumstances exist—either when my health condition may seriously jeopardize my life, health, or ability to regain maximum function, or when I am currently undergoing treatment using the non-formulary drug. The plan must make a coverage determination and notify you and your physician within 72 hours, and if approved, must provide coverage for the duration of the exigency—as long as your urgent medical condition persists or your current course of treatment continues.
Where do I mail an FEP or OPM appeal?
- Initial appeal to FEP:
- Fax (fastest): 1-877-378-4727
- Mail: Service Benefit Plan, P.O. Box 52080, Phoenix, AZ 85072-2080
- OPM escalation (if denied):
- Email (fastest): FEDCLASS_APPEALS.INTERNET@opm.gov
- Mail: U.S. Office of Personnel Management, Healthcare & Insurance, Federal Employees Insurance Operations, FEHB 1, 1900 E Street NW, Room 3425, Washington, DC 20415-3610
- Important ⚠️: Fax or email is strongly recommended. Mail can take 2-3 weeks for delivery, which could delay your decision and cause coverage gaps.
- Where can I learn more?
- FEP Blue: Dispute a claim page – summarizes 6-month window, urgent 72-hour clock, and “address on your EOB”. 
- More detail: Your Guide to Disputing a Claim – dives in on member rights, deadlines, and where to send your appeal.
The easiest way to file your FEP formulary exception request
It’s to use Claimable! We hope this guide has been useful if you’d like to go at appealing on your own. But if you’d like help, we’re here to make it quick, easy, and effective – and thanks to our partnership with Dupixent, it’s 100% free for qualifying commercial insurance members.
With Claimable, you can:
- Easily create your formulary exception request letter, in line with all of FEP’s standards and our proven formula for winning appeals.
- Source and cite the exact plan provisions and clinical precedents that strengthen your case.
- Automatically fax and mail – no downloads, no post office.
- Escalate if needed – because we’ll keep fighting for you all the way to a win.
Ready to get started? Begin your appeal here.
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!