Win more appeals with fewer headaches

Empower your patients to overcome unjust denials
Using Claimable is like having your own team of insurance experts advocating on behalf of you and your patients.
A powerful tool in your appeals kit
850 million claims are denied annually, but fewer than 1% of patients ever appeal. Not because appeals don't work, but because most patients don't know they can.
Patient appeals carry legal protections provider appeals don't, including mandated response timelines and external review rights. Their appeal doesn't replace yours – it amplifies it. Two appeals create pressure from two directions, and more opportunity to win.
Claimable gives your patients everything they need to file a strong, evidence-backed appeal on their own. More chances to get covered with less paperwork and headache for both of you.
Personalized. Robust. Fast.
Claimable’s AI-powered appeals start with your patient’s medical story and analyzes the most relevant clinical research, policy details, and legal precedents to generate truly tailored appeals - giving your patients the best chance at overturning unjust denials with less delays.

How Claimable works for patients
The Claimable experience is fast, intuitive, and fully guided, making it easy for patients to complete.



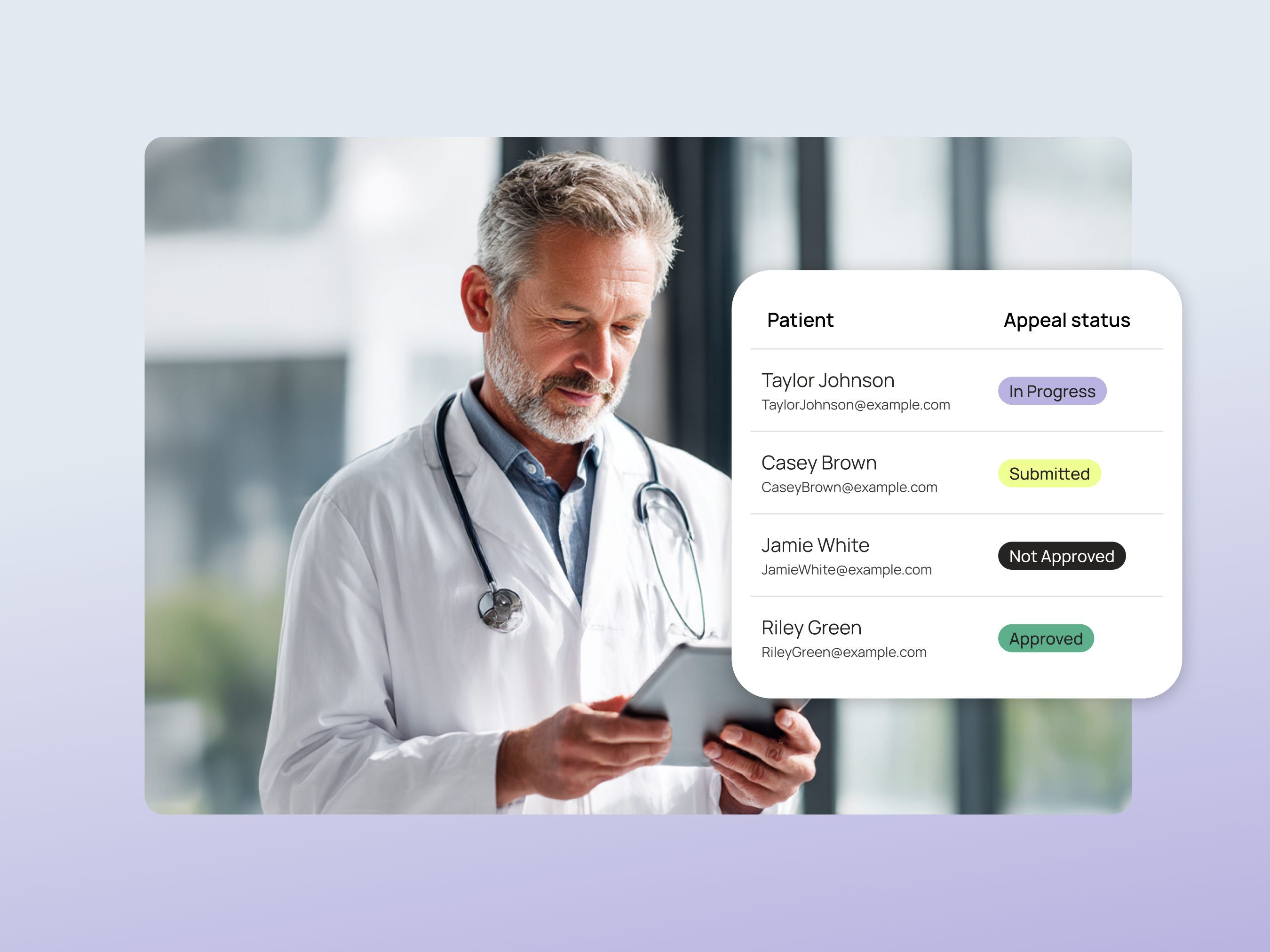
However you practice, appeal with Claimable
Claimable is designed to complement your existing workflows – not replace them. How you engage depends on your practice setting:

For independent practices appealing on their own
Request your patient referral kit below: Templates, flyers, and appeals education for everything patients need to get started.
For providers practicing in health systems
If you're a provider within a health system interested in Claimable, learn more here.
If you partner with a hub or support program
If you already work with one of these partners, contact us to learn how your patients could use Claimable through existing access networks.

No, a patient appeal does not replace your provider appeal or letter of medical necessity. In fact, the two work best together. Patient appeals are most effective when supported by a provider’s letter of medical necessity and actively promoted by the provider to their insurance contacts. We believe appeals are a team effort. Patients have legal appeal protections that can increase their chances of success, minimize delays, and reduce the burden for providers. Patients can continue appealing even if a provider’s appeal has been denied or ignored, and they often can escalate to external, independent reviewers if needed.
When discussing the option of submitting a patient appeal, it’s important to reassure your patient that they have the right and ability to advocate for their own care. Here are some steps to guide the conversation:
Empower Them: Explain that patient appeals are a powerful tool in challenging insurance denials, and that they can continue the fight even if your appeal has been denied.
Offer Support: Let them know that you’ll continue to advocate on their behalf and be available to answer questions, such as providing a letter of medical necessity.
Explain the Process: Briefly outline the steps involved in filing an appeal, and reassure them that tools and resources like Claimable are available to help guide them through the process.
Encourage Persistence: Remind them that appealing can be a process that may require persistence. However, their rights allow them to escalate the appeal if necessary.
Claimable is now available nationwide and accepts denials from all insurance providers, including Medicare, Medicaid, United Healthcare, Anthem, Aetna, Cigna, and BCBS plans. We currently support appeals for over 85 life-changing treatments, including medications for autoimmune and migraine sufferers. We will be expanding fast, launching new conditions and treatments regularly to support more people experiencing denials. Denial reasons may vary, including medical necessity, formulary exclusions, out-of-network exceptions, and site-of-care exceptions.
Affordability is central to our mission at Claimable. We charge a flat fee of $39.95 per appeal, plus shipping – and many appeals come at no-cost to patients thanks to our partner network. Patients only pay when they’re completely satisfied and ready to submit their appeal.
All of your data is handled with strict adherence to HIPAA regulations, ensuring your personal information is protected with the highest standards of security and confidentiality. Claimable uses encrypted data storage and transmission protocols to safeguard your information from unauthorized access. As a covered entity, providers must sign a Business Associate Agreement (BAA) and be verified before they can share personal health information (PHI).
Claimable crafts powerful appeals by combining your story, data, evidence, and policies with persuasive writing and validated appeal strategies to maximize success. Tested with providers and patients, and built by insurance experts, our platform continuously improves by applying insights from past appeals.
Claimable does not provide medical or legal advice, and is not a substitute for doctors or lawyers. We assist by crafting custom, evidence-based appeals that summarize relevant guidelines, policies, and regulations to help you advocate for your patient or provider rights.
Our advocacy supports:
- Patients: Empower them to protect their consumer and patient rights.
- Physicians: Support their ability to practice medicine without interference.
- Lawyers: Provide a foundation for legal action if necessary.
For legal or medical advice, please consult a licensed attorney or healthcare provide










