CVS Caremark denied Zepbound? Here’s what to do if you don't want to switch to Wegovy.

December 2025 update: This article was originally written in summer 2025 when CVS Caremark notified patients about a switch from Zepbound to Wegovy. Now, as plans renew for 2026, many people are receiving similar updates – Zepbound will no longer be on their formulary in the New Year. The good news? You can still submit a formulary request to keep coverage for Zepbound. Learn more about past formulary changes in this article, check out more on our Zepbound appeals here, or get started today.
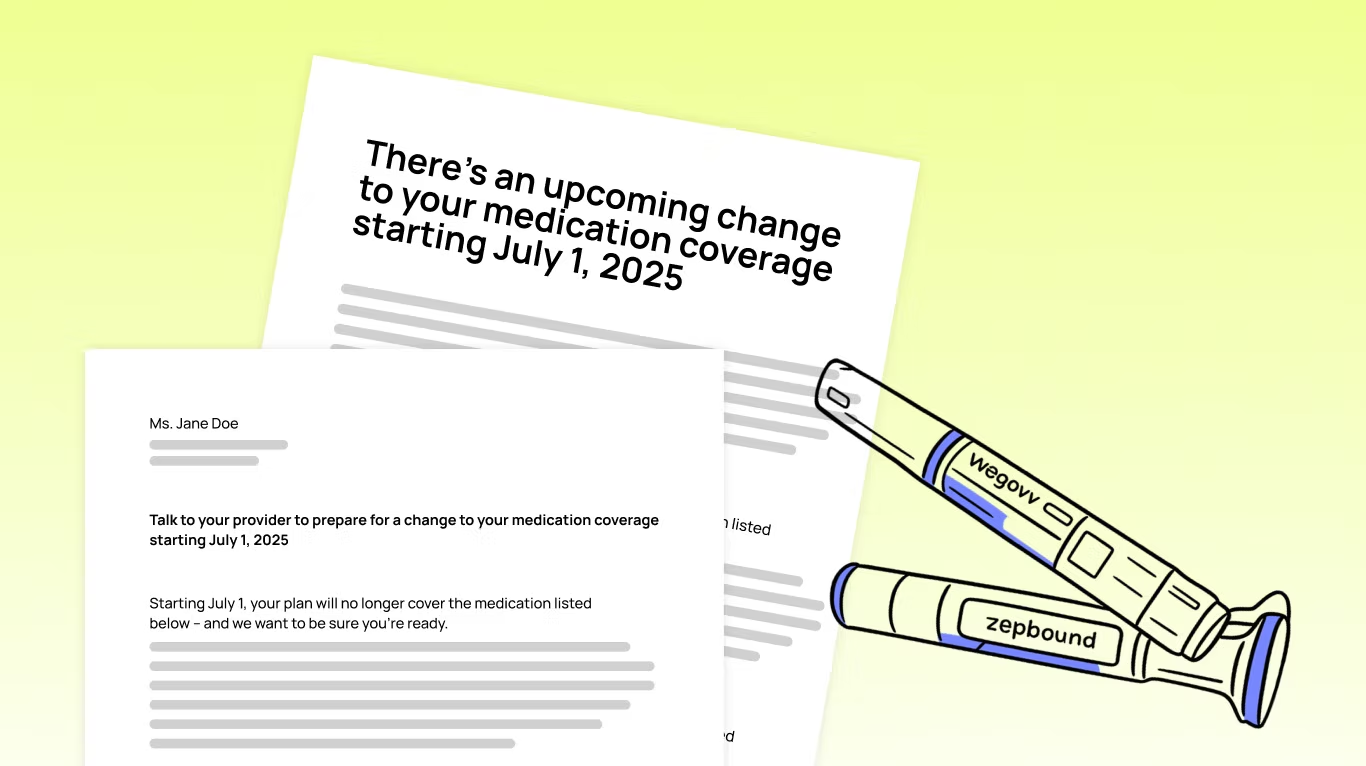
Starting July 1, 2025, CVS Caremark will stop covering Zepbound – even if it's been working for you. Thousands of patients with conditions like obesity, obstructive sleep apnea, and other conditions are being notified that they must switch to Wegovy to stay covered.
If you received a letter saying your coverage is changing, you're not alone. And you have options. What's happening here is called a "formulary change", and while it may seem final, you can appeal – and win.
At Claimable, we help people fight insurance denials every day – which means this isn't our first forced switch, and it won't be our last. Read on for our guide on what you need to know, why it matters, and exactly how to push back to stay on the medication that's working for you.
Quick Summary: What you need to know
- CVS Caremark is removing Zepbound from its formulary starting July 1, 2025
- Patients will be required to switch to Wegovy, even if Zepbound is working
- You have the right to appeal this switch, and federal law requires a decision in 72 hours
- Zepbound and Wegovy are not interchangeable – Zepbound may work better for some patients, especially those with OSA
- Claimable is building a tool to help you appeal your Zepbound denial quickly and effectively
Why is CVS Caremark suddenly denying Zepbound?
CVS Caremark, owned by CVS Health, is one of the largest pharmacy benefit managers (PBMs) in the country. They recently struck a deal with Wegovy's manufacturer, Novo Nordisk, to make Wegovy the "preferred" GLP-1 medication on its formulary. As a result, Zepbound is being dropped from coverage starting July 1, 2025, even for patients already using it with good results.
This change isn't about safety or effectiveness. It's about money. PBMs negotiate rebates with drugmakers, and these behind-the-scenes deals often determine which medication you can get – regardless of what's best for patients.

What does formulary change mean?
A formulary is the list of medications your pharmacy benefit manager (PBM) or insurer agrees to cover. When a drug, like Zepbound, is removed from the formulary, your insurance will no longer pay for it – even if it was previously approved and is working well for you.
Changes to your formulary affect your coverage – not your pharmacy. Whether you fill your prescriptions at a CVS pharmacy or elsewhere, you'll be denied coverage for Zepbound everywhere starting July 1 unless you appeal, which means it's time to understand what's changed, and make an action plan.
While Zepbound is on the out, Wegovy isn't the only GLP-1 that CVS Caremark is covering. Here's a snapshot of what CVS Caremark will and won't cover under its updated formulary:
| MEDICATION | COVERAGE STATUS |
|---|---|
| Zepbound | ❌ Not covered |
| Wegovy | ✅ Preferred drug |
| Saxenda | ✅ Covered |
| Qsymia | ✅ Covered |
| Orlistat | ✅ Covered |
| Ozempic | ✅ Covered for Type 2 Diabetes only |
| Mounjaro | ✅ Covered for Type 2 Diabetes only |
Why It Matters
Zepbound and Wegovy are not interchangeable. Zepbound uses a different mechanism of action (dual action GIP/GLP-1 receptor agonism), which means it may be more effective, and is often better tolerated – especially for people with specific conditions like obstructive sleep apnea (OSA). And older medications included on the CVS Caremark formulary – like Saxenda, Qsymia and Orlistat – are far less effective and not considered equivalent medications.
Forced switching when you've reached a stable, effective dose isn't just frustrating – it's disruptive and medically risky, potentially causing:
- Weight regain or return of symptoms
- New, intolerable, side effects
- Health setbacks and scares
- Extra clinician visits and increased costs
At Claimable, we believe your care plan should be based what's medically best for you, as determined by your doctor – not what saves your PBM money.
What to do if Zepbound is denied
If your Zepbound prescription is denied, you can file a formulary exception appeal. And in many cases, insurers are required to honor that appeal if your doctor says switching could harm you.
Here's exactly what to do.
Step 1: Get a refill before July 1
Request a 90-day refill or 30-day vacation override before July 1 (if allowed by your plan) to give you a buffer while your appeal is reviewed. This will help you avoid a care gap.
Step 2: Talk to your doctor
Reach out to your doctor now so you're ready when the July change kicks in. Ask them to:
- Be ready to file a new prior authorization for Zepbound on or after July 1.
- Write a letter of medical necessity if you decide to file your own appeal.
Step 3: File your appeal
Starting July 1, your claim for Zepbound will be denied. Once that happens:
- Submit a formulary exception request.
- This can be submitted by you or your doctor, but we recommend submitting the appeal yourself with your doctor's Letter of Medical Necessity attached. Patient appeals often have more legal rights and require responses from the insurer on faster timelines.
- This tells the insurer that Zepbound is medically necessary for you.
- Insurers must respond within 72 hours under federal law.
Less than 1% of people appeal denied claims, but those that do win about 50% of the time. You can boost your odds by following our tips below – or by using our custom tool to build the strongest possible appeal for you.
What to Include in Your Appeal
For the best chance at winning, submit an appeal letter requesting a formulary exception that explains why switching could harm you.
A strong appeal letter should include:
- Your medical results on Zepbound (weight loss, symptom control, etc.)
- Any prior medications that you've tried and failed
- Specific medical conditions like OSA that Zepbound uniquely treats
- A letter from your doctor supporting continued use
- Clinical studies, applicable laws and insurance regulations, and precedents from successful appeals with similar cases to yours
- Supporting evidence like lab results, weight logs, dosing history and medical records
Your appeal should make the case that Zepbound is working for you and that you want to avoid disruption to a stable, effective treatment plan – and be backed up by solid documentation.
Your legal rights to appeal
Under federal law, you have the right to request a medically necessary exception when a formulary change puts their care at risk.
Federal Law: 45 CFR § 156.122(c) "A health plan providing essential health benefits must have a process in place that allows an enrollee, their designee, or prescribing provider to request access to a clinically appropriate drug not otherwise covered by the plan. If granted, the plan must treat the excepted drug as an essential benefit and must respond within 72 hours." View the regulation →
On top of federal protections, many states have laws preventing insurers from forcing stable patients to switch medications mid-year. These non-medical switching or continuity of care laws may guarantee:
- You can't be forced to switch if the medication is working.
- Your doctor can override the change with a written statement.
- You must get advance notice and a clear process to stay on your current drug.
- When an exception is granted, your copay and coverage tier must stay the same.
Check here to see the non-medical switching laws enacted in your state – especially if you live in California, Illinois, Texas, or another protected state.
What to do if you get denied again
If your first appeal is rejected:
- File a second-level appeal or request an external medical review, depending on what the denial says is your next step. You have a right to multiple appeals and many people win and the second try, especially when an independent reviewer is involved.
- File a complaint with your state's Department of Insurance, especially if they refuse to give you a timely decision or fail to have a qualified clinician give you a full, fair review.
- Let your employer know—they can override the PBM if you're on a self-funded plan.
CVS has tried this before – and patients fought back
In 2022, CVS removed the life-saving blood thinner Eliquis from its formulary, forcing 150,000 patients to switch. After public outcry, provider backlash and reports of serious strokes and heart attacks, they reversed course.
We believe they can – and should – do the same here. We encourage you to consider signing the petition demanding they reverse the policy.
Create the strongest possible appeal, the easy way
From the right clinical studies to specific appeal precedents that apply to your unique circumstances, at Claimable we know how to fight – and win – forced switches like these.
Our fast, affordable tool helps you fight back. Our platform:
- Creates a personalized appeal letter backed by evidence
- Walks you through the process step by step, so you can get your appeal done in minutes, not days
- Compiles and ships your appeal not just to your insurer, but to other relevant parties like your state's Department of Insurance, HHS, and others – so your insurer knows you mean business.
Frequently Asked Questions
Does CVS Caremark cover Zepbound? No. As of July 1, 2025, Zepbound is being removed from the CVS Caremark formulary.
Can I appeal the switch to Wegovy? Yes. You have the legal right to request a formulary exception for medical necessity.
Is Wegovy the same as Zepbound? No. Zepbound uses dual GIP/GLP-1 action and may work better for some patients.
Will Medicare cover Zepbound? Aetna Medicare plans often exclude weight loss drugs like Zepbound. Appeals here may be more difficult, but not impossible.
Final Word: Your Care. Your Rights.
If Zepbound works for you, you have every right to fight for it. Forced switches driven by rebates, not results, are wrong. Claimable is here to help you fight back.
Start your appeal now to protect your care.
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!