Close the access gap

10
DAYS
AVG RESPONSE
3x faster resolution gets
patients back on therapy faster
OVER
80%
WIN RATE
1.7x industry average in established conditions
15+
HOURS
SAVED PER APPEAL
Reduce the time and cost
it takes to appeal
$20+
MILLION
UNLOCKED VALUE
Appeals proven to work
even in complex specialties
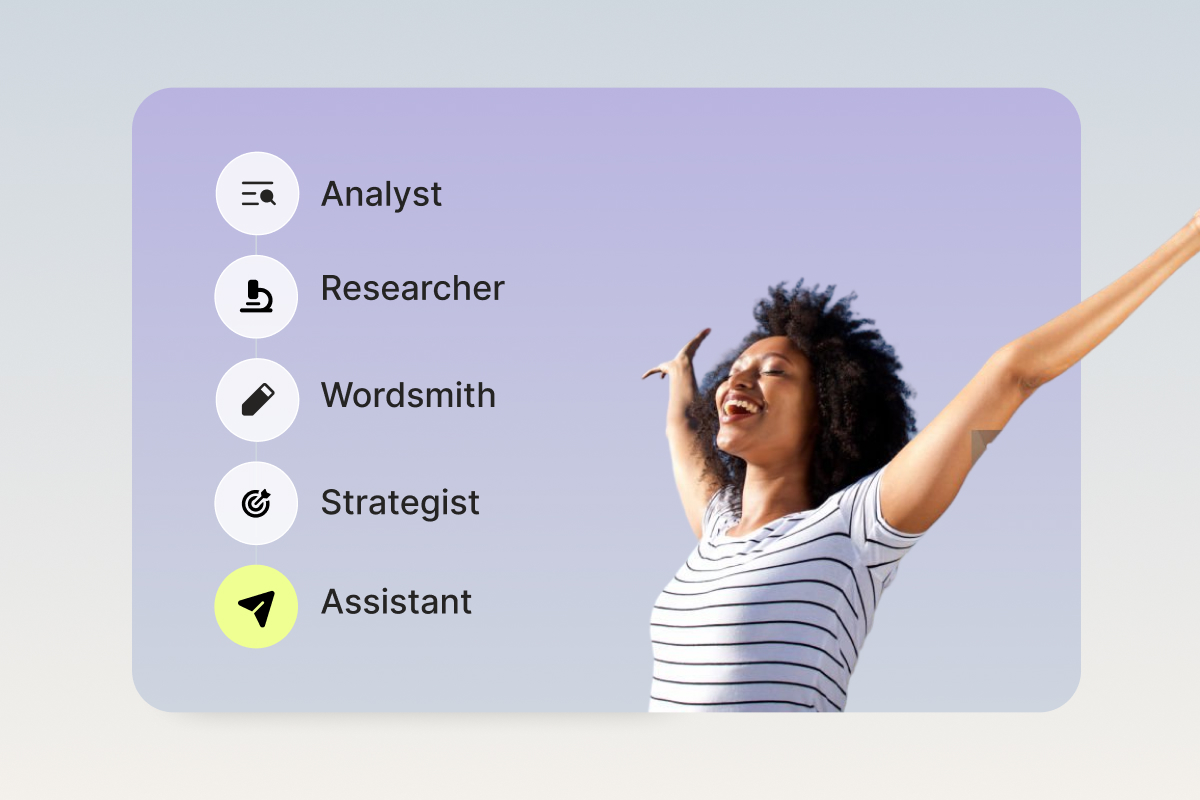
Automate appeals with Claimable
Denials are now automated and intelligent.
Your defense should be too.
HIPAA-compliant appeals solution
Claimable combines the legal force of patient rights with support team tools to appeal with scale, speed, and cost efficiency.
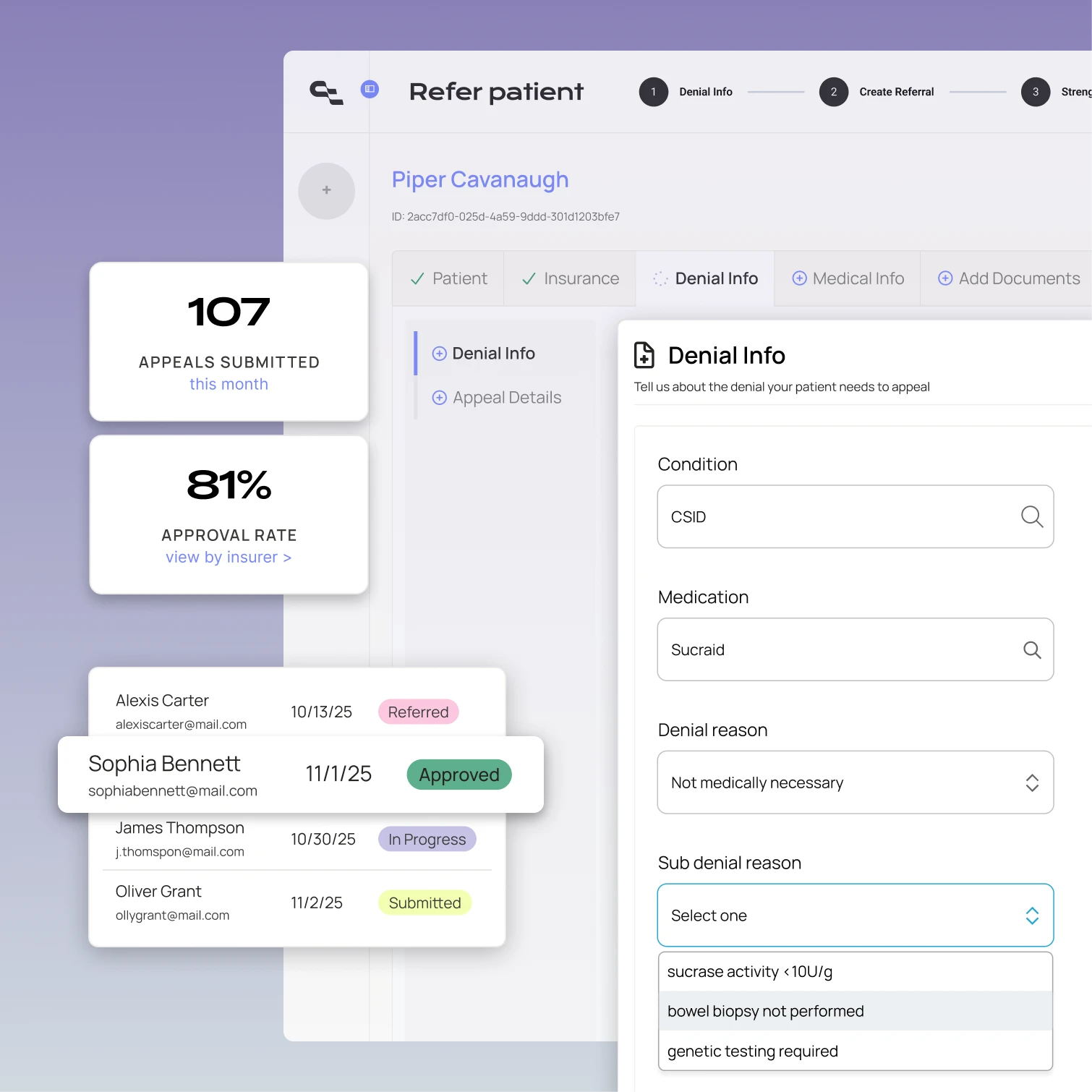
Support teams and patients work seamlessly in our easy web app.
Upload docs, add details and create strong appeals in minutes, not hours.
Seamlessly track appeals progress and outcomes in one view.
Monitor success rates by payer, state, therapy and denial type.
Scale without constraints
Self-service patient experience and automation remove support team capacity constraints, so you can appeal every denial – even as rates rise.
✓ Seamless patient intake via web app or API
✓ Generate high-quality appeals in minutes
✓ Support team or patient-led options
Proven to win complex cases
Fueled by a purpose-built database and proprietary AI model, Claimable appeals offer your patients the best and most likely path to coverage.
✓ Fully customized to denial reason, condition and insurer
✓ Constant learning to beat new denial tactics and win more
✓ Faster, more effective than provider programs alone
Strategic intelligence
Finally, denial insights that move your business forward. Analyze denial rates by insurer, state, therapy, denial reason and more – and get the data to understand your patient support impact.
✓ Custom dashboard for the insights you value
✓ Understand impact per appeal and brand
✓ React faster to combat new denial strategies


We work how you work
Connect your hub, specialty pharmacy, or in-house team to Claimable to make appeals seamless and easy. From quick-start options to direct API integrations, we plug in where you need us.
✓ Customize Claimable to fit your team's workflow
✓ Plug-and-play tools to bespoke integrations
✓ Support materials for teams, FRMs, and patients
Compliance you can count on

Getting started is easy
Launch in as little as 2 weeks
1
2
3
See Claimable in action
Download a sample appeal
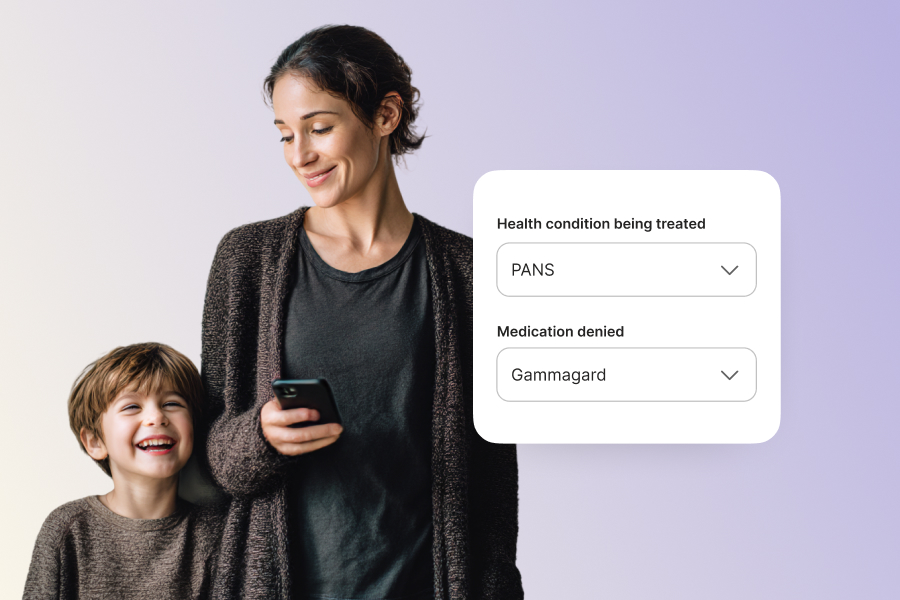
How Claimable's AI works for patients
Patient-led appeals usually carry more leverage and legal protections than provider-led ones.
They trigger patient rights.
When the patient—not the provider—files the appeal, it activates mandated timelines (often 72 hours), qualified (human) reviewer requirements, access to insurer documents, and the option for independent external review. These protections often don’t apply to provider submissions.
The patient holds the contract.
Insurance coverage is a legal agreement between the patient and their plan. Providers focus on clinical need, but patients can also assert contractual and legal rights—making the case stronger.
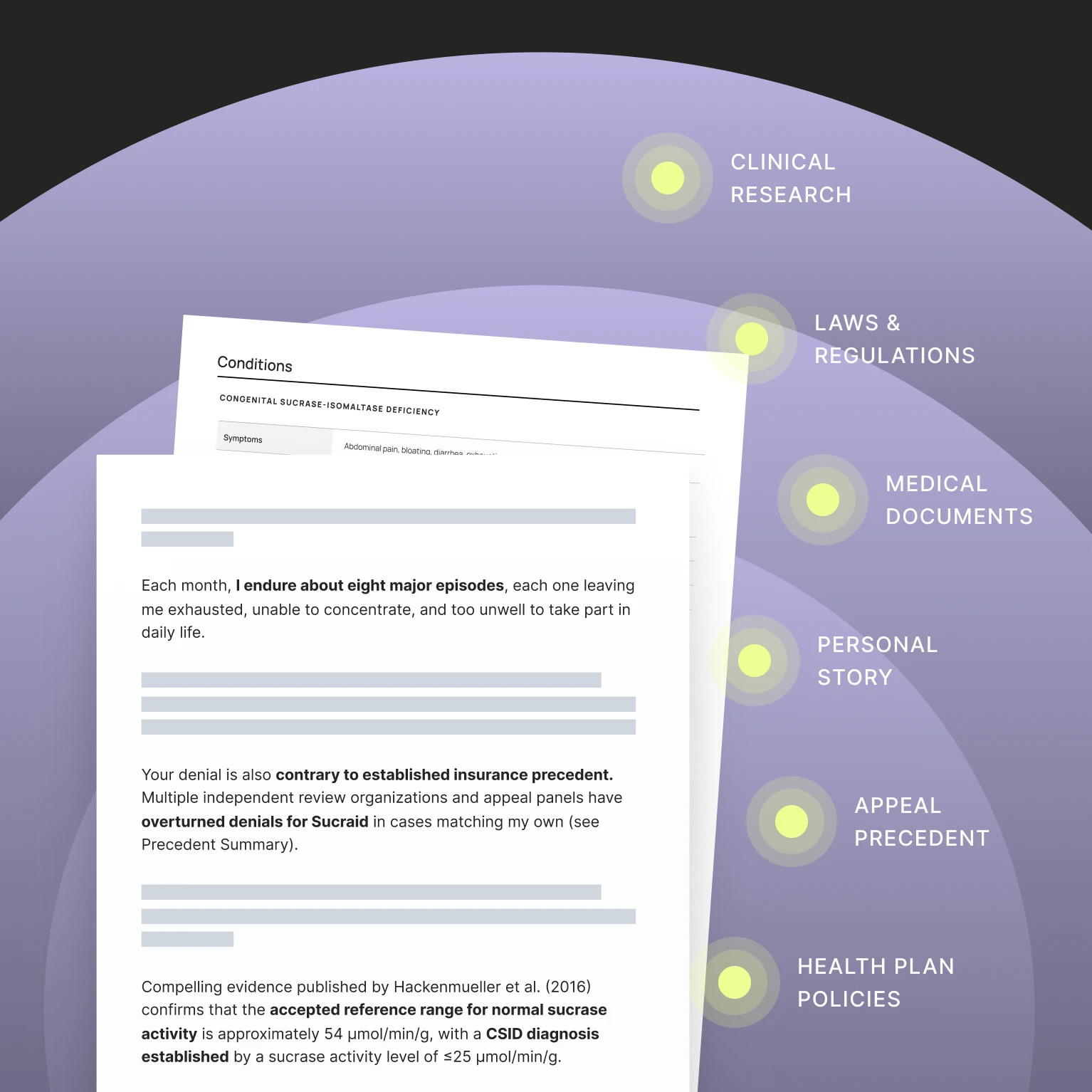
They create a more complete appeal.
Provider appeals are typically short clinical notes. Patient-led appeals can combine the physician’s justification with clinical research, policy arguments, legal references, and personal impact—resulting in a more persuasive submission.
More denials actually get appealed.
Only 18% of physicians have capacity to appeal—limited by staff constraints for paperwork and peer-to-peers, and 46% of patients abandon treatment after a denial. Patient-led appeals close this gap and scale far more efficiently than traditional hub or PSP processes.
And they work.
Claimable’s patient appeals have an ~80% success rate for established conditions, with most approvals in under 10 days—helping more patients access necessary treatment faster.
Traditional manual appeal processes for initial, second-level and external appeals are costly, requiring proportional headcount increases as denial volumes rise. Claimable's AI-powered platform fundamentally changes this equation through three key mechanisms:
Scale without staffing: Self-service patient intake and automated appeal generation eliminate capacity constraints. Appeals that once took hours are now completed in minutes, with no additional headcount required as volumes increase.
Quality that wins: Our AI doesn't just generate generic appeals—it integrates condition-specific clinical evidence, payer policy analysis, state-specific legal requirements, and the patient's personal story into comprehensive appeals that achieve 80% approval rates. The system continuously learns from outcomes, and our appeal experts adapt strategies to improve performance over time.
Strategic efficiency: By reducing appeals from 15-30 hours of manual work to minutes of automated processing, cost per appeal decreases dramatically while maintaining the clinical rigor and legal precision that win cases. Real-time visibility and analytics enable continuous optimization impossible with quarterly vendor reports.
The result: Pharmaceutical companies can scale appeal support to match rising denial rates without the linear cost increases that make traditional programs unsustainable.
Yes. Claimable is designed for flexible integration across diverse operational models, from exclusive specialty pharmacy relationships to multi-vendor hub environments.
For specialty pharmacy partnerships: When you have an exclusive specialty pharmacy relationship, Claimable can embed directly into their workflow through our secure Appeals Hub. Pharmacy concierge staff access the platform with a Business Associate Agreement (BAA) in place, enabling them to manage cases, make referrals, and track appeal status in real-time. Patients are then invited through direct referral or self-enrollment via branded landing pages.
This model creates significant value because exclusive specialty pharmacies see 100% of patients for a given product, already maintain high-touch relationships, and share aligned goals around faster, more successful appeals.
For hub services vendors: Claimable integrates through API-driven architecture or simple referral links, requiring no heavy IT lift. We support both embedded workflows (where hub vendors incorporate appeals into existing patient journeys) and standalone models (where appeals become a distinct service line).
For multi-pharmacy environments: When products flow through multiple specialty pharmacies, Claimable standardizes the appeal experience while maintaining flexibility for pharmacy-specific workflows. This is particularly valuable in the "walk" phase of program maturity, where consistency across channels becomes critical.
Implementation approach: We customize integration based on your program reality—starting with simple pilots for new programs ("crawl"), expanding to multi-channel standardization ("walk"), and ultimately automating data transfer for scale and efficiency ("run").
Claimable launches in weeks, not months. Most partners define requirements and approvals in the first 1–2 weeks, configure and test in weeks 3–4, and go live by weeks 5–6. Timelines vary based on degree of customization, complexity of workflow or system integration and content approval processes. Because implementation doesn’t require heavy IT lift—setup can be quick and low-friction.
Our team provides a proven playbook, handles configuration for your therapies and indications, and trains your support teams before launch. Once live, patients can begin generating appeals immediately, and partners typically see their first successful appeals within 2–3 weeks, with full program optimization within 90 days.
Appeals data creates a new category of leverage in payer negotiations by documenting systematic denial patterns, demonstrating the burden imposed on patients and providers, and proving the medical necessity of coverage.
Denial pattern intelligence: Claimable's aggregate analytics identify which insurers or PBMs deny most frequently, for which indications, using which denial reasons, and with what success rates when appealed. This transforms contract discussions from theoretical debates about coverage policy to fact-based conversations about actual insurer behavior.
Quantified patient impact: Real-world data showing how many patients abandoned treatment due to denials, how long appeals took, and what financial burden patients faced creates compelling evidence for contract terms that reduce administrative friction.
Medical necessity documentation: High overturn rates (80%+ in our established programs) demonstrate that denials are often inappropriate, not medically justified. This evidence supports arguments for coverage expansion, prior authorization elimination, or expedited review processes.
Comparative leverage: When you can show that Payer A denies at 2X the rate of Payer B for the same indication, you create competitive pressure and negotiating leverage for improved terms.
Strategic applications:
- Negotiate lower prior authorization requirements for proven indications
- Establish expedited review pathways for time-sensitive therapies
- Secure reasonable coverage criteria based on FDA and clinical guidelines
- Build case for preferred formulary positioning
Market access teams using Claimable data can make payers take denial patterns more seriously when confronted with systematic evidence versus anecdotal complaints.
Claimable maintains healthcare-grade infrastructure with comprehensive compliance frameworks:
- Infrastructure & Certifications: Claimable runs on HIPAA-compliant, AWS-hosted infrastructure with BAAs in place, is HIPAA certified by Workstreet (November 2025), and is actively pursuing SOC 2 Type II certification (expected December 2025).
- Access Controls: We use strict role-based access, MFA, and full audit logging to ensure only authorized personnel access PHI.
- Data Handling: All data is encrypted in transit and at rest, supported by automated retention/deletion policies and regular security testing.
- Patient Consent & Controls: Patients receive clear, plain-language consent disclosures, can review and revise appeal inputs and outputs, can control who accesses their data, and may revoke access or request deletion at any time.
- Governance Framework: Our Privacy/Security Officer oversees rigorous policies for access management, incident response, vendor oversight, and human review of all AI-generated content.
- Vendor Assessment Support: We provide detailed security documentation, complete questionnaires, and support IT reviews to meet pharma and enterprise compliance requirements.
Our approach aligns with common infrastructure standards in pharma, emphasizing being innovative yet low-risk for enterprise clients.
They can work sequentially or in parallel, depending on urgency and program goals.
- Sequential (provider first, patient second): Ideal when payers require HCP input or when complex clinical evidence is needed. The provider appeal establishes the medical case; the patient appeal follows with contractual, legal, and impact-based arguments when initial provider appeal is unsuccessful.
- Patient-first: Useful when provider capacity is limited or when the medical literature is clear. The patient leads with a comprehensive case incorporating provider documentation.
- Parallel: Best for high-stakes or time-sensitive therapies. Provider and patient appeals submit complementary cases at the same time to maximize pressure and shorten delays.
Across all models, Claimable coordinates submissions to keep messages consistent and ensure patients’ contractual and harm-based arguments strengthen—not duplicate—the medical case.
Claimable uses a human-in-the-loop model, meaning patients stay fully in control of their appeal. The system guides users through intake, generates a draft using curated evidence, and requires patients to review and approve everything before submission.
How it works:
Patients provide their medical and denial details through a guided intake. Claimable drafts the appeal using clinical, policy, and legal evidence matched to their case. Patients verify accuracy, make edits, and authorize submission—nothing is sent without their approval.
How we prevent errors:
We use constrained, expert-curated evidence sources to avoid AI hallucinations. Patients complete clear verification steps to confirm accuracy. Eligibility checks, LLM observability and evaluation, expert oversight, and outcome learning continuously improve quality and safety.
What this isn’t:
Claimable doesn’t replace medical judgment or submit appeals automatically without review. Patients remain the decision-makers, and AI simply structures their story with supporting evidence.
For sponsored programs:
When Claimable is offered at no cost through a manufacturer, patients are informed clearly during consent. This maintains transparency and appropriate boundaries.
Claimable is the only AI platform built specifically for fighting unjust insurance denials—designed for accuracy, safety, and the real human impact behind every case.
Unlike lightweight GenAI or one-size-fits-all tools, Claimable:
- Puts the patient story at the center of every appeal to highlight the real-world consequences of losing coverage.
- Uses expert-curated clinical, policy, and legal evidence that is recent, relevant, reputable, and validated.
- Matches evidence to the exact treatment-and-condition pair, avoiding the errors common in generic AI tools.
- Evaluates insurer errors, policy violations, and patient rights, including compliance with medical policies, benefit rules, step therapy laws, and federal protections.
- Tailors each appeal using over a million strategy combinations, instead of relying on generic, flat templates that insurers can disregard.
- Automates fax and mail submission using a proprietary addressbook of payer decision-makers, regulators, decision-influencers and escalation targets.
- Never leaves users at a dead end, always providing a concrete next step—second-level appeals, external review, OPM, ERISA rights, employer escalation, or state regulators.
- Is designed to work with enterprise businesses, with privacy, security, auditability, and compliance safeguards built for regulated healthcare environments.
Let’s Work Together
Schedule a call to see the difference Claimable can make. Here’s what we’ve achieved together with brands like yours:









