Resources
Latest Posts

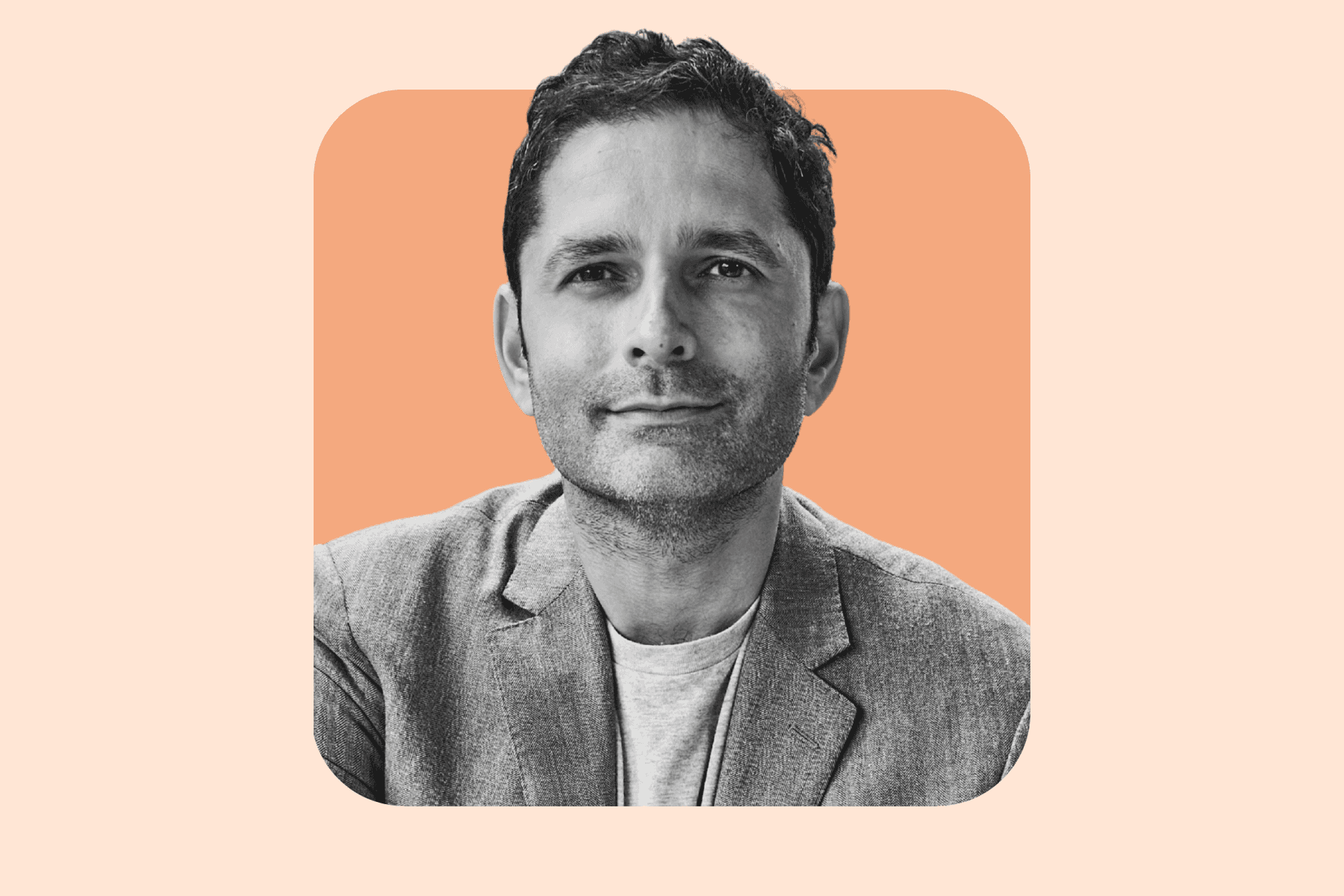
Claimable's CEO, Warris Bokhari, MD, shares Claimable's mission to challenge denials in an open letter to celebrate our launch.
Providing healthcare to a population as diverse as ours is no easy task. It requires balancing evidence-based science, cost-effectiveness, and scalable delivery. Ultimately, it’s about empowering doctors to do what’s right for their patients.
However, as a doctor, former healthcare executive, and someone living with a chronic condition, I’ve seen firsthand that the US healthcare system is often a business first and focused on patient care second.
It’s also infested by middlemen businesses that drive up costs and block access. After decades of working within and examining the healthcare system, I became determined to understand where things went wrong—and more importantly, how to make them right.
The more I dug in, one thing became abundantly clear: better patient care often doesn’t align with bigger business incentives. Too often, short-term profits are prioritized over patient lives, provider autonomy or even long-term healthcare savings. This imbalance deeply troubled me.
As someone who's spent years developing patient care models, I’ve seen that getting results takes time—lots of it. You come up with a hypothesis, test it, and if it works, hope someone turns it into a product. On the flip side, success in the U.S. healthcare system seems to be defined as managing and defending payments rather than helping patients. For example, in the last decade, we’ve seen telehealth companies come and go, while risk adjustment companies in the medicare advantage space have raised vast amounts of money without producing better patient outcomes.
After almost a decade working in big corporations, I realized that the industry wasn’t just failing patients, it was actually working against them, making it hard for them to get the care they deserved. One of the biggest barriers? Denials. I was shocked by the numbers: 850 million claims denied each year? 1 in 5 people impacted? This seems unbelievable, but it’s real.
In the insurance world, denials are often blamed on "fraud, waste, and abuse." But is that really the whole story? In exploring the concept for Claimable, I started talking to people facing denials and heard countless horror stories of essential care being rejected without clear explanations or alternatives.
What struck me most was this: when people do appeal, many of these denials get overturned. But here’s the problem—almost no one actually appeals.
I knew from my time inside that insurers aren’t really hearing the stories of people they deny care to. My gut told me this was the start of a hidden public health crisis.
At that point, I knew something had to change, but I couldn’t do it alone. That’s where my co-founders, Alicia and Zach, came in and Claimable came to life. I’ve always loved working with people who are smarter than me—it pushes me to think outside the box and lean into more of a creative space.
Alicia, Zach, and I were united in wanting to solve real problems, along with a sense of impatience about the pace of change in the healthcare industry. We see a (somewhat) straight line between where we are and a better world, but the path is not an easy one. We’re rowing against the tide of traditional healthcare, going up against an industry that’s comfortable making a lot of money the old way.
But we’re all driven by the same goal: to fix real problems in healthcare and help pave the way for true innovation.
We’re also bound by personal experiences that led us here. In my case, having been raised by two disabled parents and having practiced medicine in the UK where patients never got denied, I deeply understand the importance of accessible healthcare. For Zach, access to care is as critical as the care itself. Driven by his passion to eliminate healthcare barriers, he spent years at the VA improving care for veterans. And Alicia, as the child of a nurse, became relentlessly curious about reimagining healthcare experiences and finding the best way to fix them.
Ultimately, what unites us is a sense of optimism. We genuinely believe the system can be better, and we’re willing to prove it. We’re not afraid to be told we’re wrong, but we’ll keep doing the work to make sure we’re right.
In the past few months, we’ve been fortunate to work directly with patients and provider groups. We’ve gotten to know their stories and we’ve deeply felt their wins, their losses, and their tragedies. We’ll never forget the migraine sufferer who became functionally disabled after years of stability, losing their ability to work when their care was suddenly denied. And we’ll always be grateful to the practice manager who inspired us with her social advocacy campaigns and her decision to become our first customer, leading to the first of many successful appeals.
All of this keeps us moored to our mission. It sets the tone for everything we do - from the culture inside the company and empathy embedded in the experiences we build, to the quality of the data we use and our passion for seeking continual improvement.
We’re focused on building a future where patients come first—not payment models.
Our mission is clear: ensuring everyone gets the care they need and the coverage they deserve.
Thanks for coming with us on this journey.
Warris Bokhari, MD

February 11, 2024 UPDATE: We are seeing an increase in denials following the recent AAP report on PANS/PANDAS. Although the December 2024 report states, "Because they are limited by the present level of evidence on the topic, the findings are presented as a report rather than a clinical practice guideline," insurers are citing it as a guideline to justify denying previously approved care. Our team is actively collaborating with experts to refine appeal strategies in response to these challenges.
Re: Selective Interpretation of PANS/PANDAS Evidence
January 31 2025
Warris Bokhari
Claimable Inc.
To the Editors:
I just finished reading the AAP's report on PANS, and while it is thorough, it raises several significant concerns that I believe warrant attention:
First, the report does not list any authors beyond the board, nor does it identify the individuals or institutions consulted as experts. This omission is unusual and raises questions about whether true expertise in managing this complex condition was adequately represented.
Second, the diagnostic pathway outlined is so intricate that it seems unlikely most insurers will provide coverage, putting families in a precarious position where they cannot exclude significant negatives and thus unable to access necessary care.
Third, while the report criticizes existing studies for being small, this critique seems misplaced. Given the relatively low incidence of PANS/PANDAS in the population, small sample sizes are to be expected in research on rare diseases. Nevertheless, I have come across numerous studies using standardized instruments that demonstrate measurable improvements in affected children.
Finally, I am concerned that the evidence review stops in 2023, excluding important recent studies like Melamed et al. (2024), which demonstrated the benefits of IVIg treatment on psychometric tests related to OCD. In addition, Melamed et al. (2021) previously published a larger open-label study showing IVIg’s effectiveness in alleviating symptoms. Given the timing of this report and the significance of these findings, it is puzzling that they were not included, particularly since position papers like this remain valid for five years.
In summary: I am deeply concerned that this position paper will be used by insurers to justify sweeping and irreversible denials of care, leaving many families unable to access treatment. The concern in the PANS/PANDAS communities among families based on this highly selective interpretation of the existing evidence.
While I recognize the limitations of small studies in this field, such limitations are common in rare disease research. The strong stance taken by the AAP could have serious implications, limiting access to the care that children with PANS/PANDAS urgently need.
Sincerely,
Dr. Warris A. Bokhari, M.B., B.S.
Submitted on January 31 2025
Featured stories
In the news
Download a winning sample appeal
Want to see what it takes to successfully overturn a health insurance denial? Download our sample appeal to learn how we build strong, evidence-based cases that get results.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Each month, I endure about eight major episodes, each one leaving me exhausted, unable to concentrate, and too unwell to take part in daily life.
The frequency and unpredictability of these symptoms have isolated me socially and limited my capacity to take part in activities most people take for granted.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!

One of our core principles is to help patients protect their rights and level the playing field with their insurance company. This includes rights to multiple appeals, fair reviews, decision rationale, exceptions when needed, and adequate network access, among others. For more, read our post on patients rights.
Claimable’s AI-powered platform analyzes millions of data points from clinical research, appeal precedents, policy details, and your personal medical story to generate a customized appeals in minutes. This personalized approach sets Claimable apart, combining proprietary and public data, advanced analysis and your unique circumstances to deliver fast, affordable, and successful results.
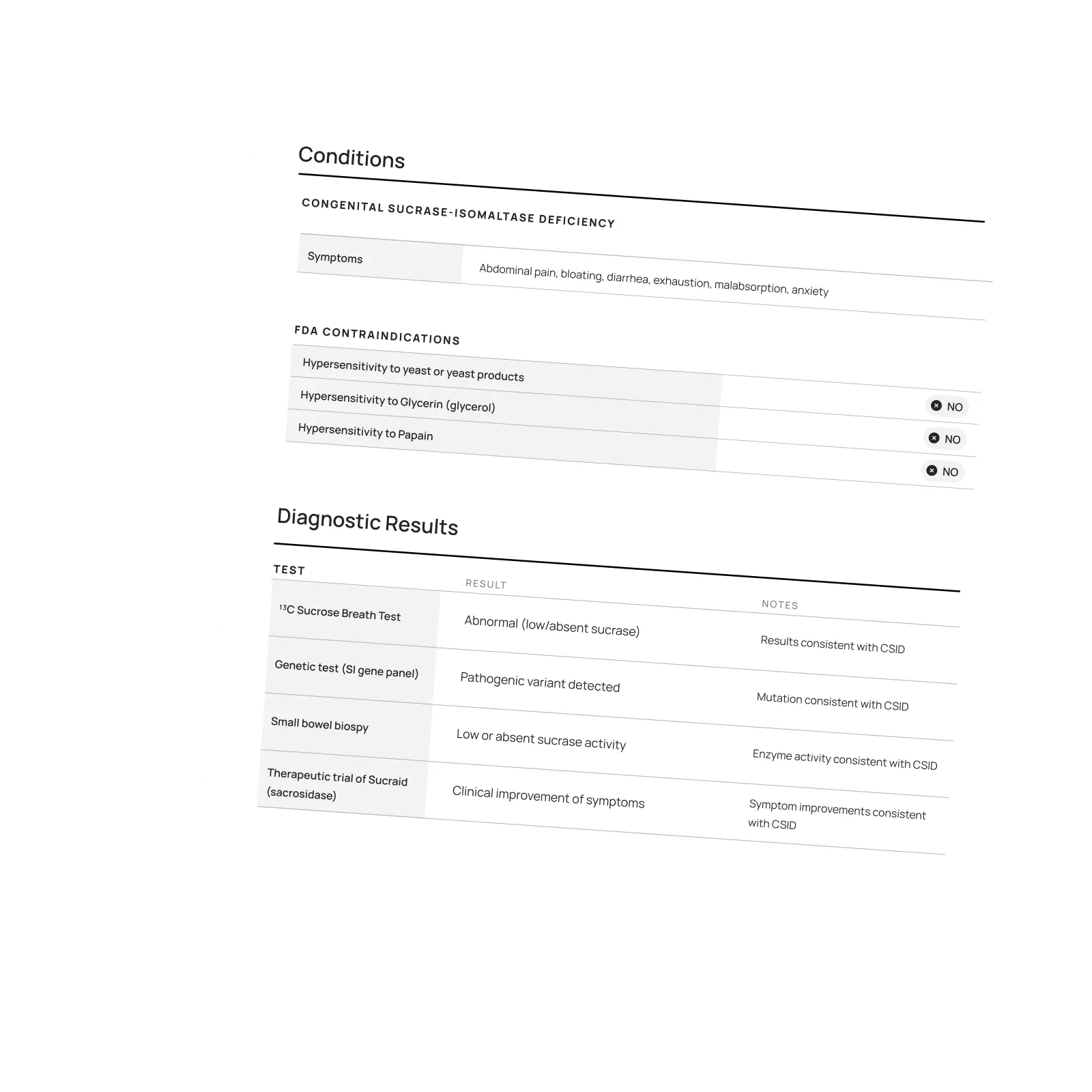
We currently support appeals for over 85 life-changing treatments. Denial reasons may vary from medical necessity to out of network, and we even cover special situation like appealing plans that won’t count your copay assistance towards your deductible (hint: those policies were banned at the federal level in 2023). That said, we are rapidly growing our list of supported conditions, treatments and reasons. You can quickly check eligibility and ask to be notified when your interest becomes available. It helps us know where to focus next 🙂
We think about appeal times in a few ways. First, many professional advocates and experienced patients spend 15, 30 or even 100 hours building an appeal–but with Claimable, this takes minutes. We automate the process of analyzing, researching, strategizing and wordsmithing appeals. Next, there is the process of figuring out where you will send it (hint: expand your reach beyond appeal departments), then printing, mailing and/or faxing your submission. We handle that, too. Finally, there is the time it takes to get a decision. We request urgent reviews when appropriate, and typically receive standard appeal decisions within a couple weeks.
Review periods are mandated by applicable laws, from 72 hours for urgent, 7 days for experimental, 30 days for upcoming and 60 days for received services. Our goal is to get a response as fast as possible, since most of our clients are experiencing long care delays or extreme pain and suffering.
Claims are denied for a variety of reasons, many of which blur definitions. We focus on helping people challenge denials by proving care is needed and meets clinical standards, in addition to addressing specific issues like experimental treatments, network adequacy, formulary or site of care preference exceptions. We don't support denials for administrative errors or missing information, as we think those are best handled by simply resubmitting the claim in partnership with your provider. That said, many of our most rewarding successes have been cases previously though 'unwinnable', with providers and patients who fought tirelessly for months without appropriate response or resolution.
A denial letter is a formal notice from your insurance company explaining why a claim was denied and how you can appeal the decision. Sometimes the notice is included within an Explanation of Benefits. It is a legal requirements; if you didn’t receive one, contact your insurance company.
A letter of medical necessity is a statement from your doctor justifying why a specific treatment is critical to your care and/or urgently needed. You can attach it to your patient appeal to strengthen your case, especially if you are requesting an urgent appeal or need to skip standard ‘step therapy’ requirements. That said, we don’t require them and are often successful without them.
A claim file contains all the documents and communications your health plan used to decide whether to approve or deny your claim. Most health plans are legally required to share this information upon request. According to a ProPublica investigation, reviewing your claim file can help expose mistakes or misconduct by your health plan, which can make your appeal stronger.
Your insurer is required by law to give you written information about how to appeal, including the name of the company that reviewed your claim and where to send your appeal. Your health insurer may work with other companies, such as Pharmacy Benefit Managers (PBMs), Third-Party Administrators (TPAs), or Specialty Pharmacies, to manage your claims. These companies might be responsible for denying your claim and handling the appeal process on behalf of your insurer.
If you don't win your first appeal– don't give up! Many people are successful on their 2nd, 3rd or even 4th try, and future appeals are reviewed by independent entities. That said, we wrote a whole guide to understanding your options, including escalating your appeal and seeking other assistance for covering costs, forgiving debt or even seeking legal or regulatory support.
While both denial rates and appeal success rates vary widely by the type of health plan, state, and insurance company, studies have shown more than 50% of people win their appeal–and we apply strategies to boost your chances of success. Claimable has an 80% appeal success rate. The biggest denial challenge is that most people never appeal–allowing unjust denials to control their healthcare options because they are unaware of their rights or lack the support needed to fight back. No one needs to fight alone–Claimable is here to help. We know first hand that many denials are based on errors, inconsistencies or auto-decisions, and have proven strategies for fighting back against this injustice.
Let’s get you covered.