Resources
Latest Posts
Learn why your health insurance claim file is essential for appealing denied claims, how to request it, and what to look for when reviewing it to strengthen your case.
What is a Claim File?
A claim file contains all the documents and communications your health plan used to decide whether to approve or deny your claim. Most health plans are legally required to share this information. According to a ProPublica investigation, reviewing your claim file can help expose mistakes or misconduct by your health plan, which can make your future appeals stronger.
When Should I Request My Claim File?
You can request your claim file anytime after a denial, but we recommend doing so if your first appeal is unsuccessful. This way, you can avoid delays or extra paperwork that might interfere with a timely reconsideration. It's a smart move to have this information in hand if you need to take further steps.
Why are Claim Files Important?
Your claim file gives you insights into why your claim was denied and may reveal errors or inconsistencies that can help you in your next appeal.
Most health plans are required to provide your claim file within 30 days, so you can review it carefully.
How to Request Your Claim File
- Request Your Claim File
If you appealed through Claimable, don’t worry—we’ve already requested it as part of your appeal process. If not, you can use ProPublica's handy template to request it yourself. - Call to Follow Up
Call your insurance company’s member services team (the number’s on your insurance card) to make sure they’re processing your request. It never hurts to check in! - File a Complaint
If your insurer doesn’t provide your claim file within 30 days, it’s time to file a complaint with your state or federal regulatory agency. You’re entitled to this information.
How do I review my claim file?
Reviewing your claim file might seem daunting, but with the right checklist, you can spot important details.
Look for any missing documents or internal communications that could reveal mistakes or issues with how your claim was handled.
And remember—you can always share your claim file securely with us at Claimable if you want to participate in our ongoing research on denial issues. Just reach out at support@getclaimable.com, and we’ll send you a secure link.
Claim File Checklist
Here’s what you should look for when reviewing your file:
Does it cover the right time frame?
It should include documents leading up to, during and after your denial. If documents provided do not cover the time period stated in your claim file request–it’s incomplete.
Does it include call recordings, transcripts and call logs?
The file should contain all phone call recordings, transcripts and/or summary logs related to communications about your claims and/or denials. If you know you or your health provider called the health plan and don’t see it in the log–it’s incomplete.
Does it include email communications?
It should include emails relevant to the denial(s), including internal messages and communications with healthcare providers. If you know you or your health provider emailed the health plan and don’t see it in the file–it’s incomplete.
Does it include internal messages?
The file should include internal communications among health plan staff about the evaluation or discussion of the denial(s). If the internal reasons or evidence differ from the denial notice, you may have strong grounds to challenge the decision.
Does it include claim approval and/or denial letters?
The file should include all formal and informal notices sent to you or your healthcare provider, such as denial letters or explanation of benefits. If the denial reasons change, you may have strong grounds to challenge the decision.
Does it include prior authorization requests and responses?
The file should include documents related to requests for authorization and their subsequent approvals or denials. If it includes medical records that were subsequently re-requested or ignored, you may have strong grounds to challenge the decision.
Does it include internal memos or reports?
The file should include any written reports or memoranda related to the denial(s) that were sent by or received from health plan staff. Look for any inconsistencies between these communications and your denial.
Final Thoughts
Your claim file is a powerful tool—it can give you the information you need to fight back and strengthen your appeal. We know dealing with denials can be frustrating, but Claimable is here to help. Don't hesitate to reach out if you have questions or need guidance.

If your insurer hasn't responded to your appeal, discover how to check status and enforce review deadlines.
We know how frustrating it is to feel ignored by your insurance company, especially when your health is on the line. But you don’t have to wait endlessly—your insurer is legally required to review and respond to your appeal within set timelines.
If you haven't heard back about your appeal–here's how to hold them accountable and make sure they stick to their deadlines.
Quick Summary – More details below:
- Call member services for a status update—you deserve quick answers.
- Use the tips below to get results and avoid delay tactics.
- If you're being ignored, file a complaint with their regulator—they’re there to help!
"Never give in, never give in, never, never, never, never—in nothing, great or small, large or petty—never give in except to convictions of honor and good sense."
–Winston Churchill
How long does my insurer have to review my appeal?
The Affordable Care Act and ERISA regulations set strict rules for how appeals are handled: who reviews your appeal, how and when they must share decisions, and the specific timelines they must follow. Below are the general review timelines, but be sure to check your denial letter for specifics to your plan.
Below are the required timelines for various types of appeals.
• Expedited Service: 72 hours
• Experimental Service: 7 days
• Prior Authorization: 15 days
• Upcoming Service: 30 days
• Received Service: 60 days
You can request an expedited appeal if waiting for a claim decision may put your health at risk, such as if you urgently require medication due to a risk to health or severe pain, or are currently in the hospital. Formulary exceptions also qualify for 72 hours reviews, when you request a treatment not covered by your plan because it is medically necessary.
How do I know when my appeal was received?
We submit your appeal via Fax and First-Class Mail with tracking to ensure delivery. You’ll receive an email receipt confirming when your appeal was faxed, and mail delivery typically takes 3-5 days. If there’s an issue with delivery, we’ll let you know and work on alternative methods. If you need a detailed tracking report–reach out to support@getclaimable.com.
How can I find out my appeal status?
Call the member services number on the back of your insurance card and ask for an update on your appeal. Sometimes your provider may receive updates faster, so it’s worth checking with them too.
Can Claimable contact my insurer for me?
Your appeal is 100% yours—Claimable helps you create and send it, but we don’t contact your insurer directly or receive updates on your behalf. Because of this, you, in addition to your health provider, will be the ones to receive any updates or decisions from your insurance company.
How Can I Check My Appeal Status?
Unfortunately, insurers often use delay tactics to avoid processing appeals. Here’s how to handle common excuses:
They say: “We never received your appeal.”
You say: “I have proof it was received on [date] at [fax number] and on [date] at [address]. Please check again. I’ve also copied regulators, your CEO, and other decision-makers. Let me know if you need a detailed tracking report.”
They say: “We need more time to review.”
You say: “No, unless you can provide a valid reason in writing today that meets legal criteria for an extension. The law requires a decision within [review days], and I’ll file a complaint with [regulator] if there’s no compliance.”
They say: “You can’t appeal.”
You say: “Under the Affordable Care Act (or ERISA for self-funded plans), I have the right to appeal, including requesting exceptions to plan policies like step therapy or formularies when medically necessary. I am entitled to my own internal and external appeals, in addition to any requests or appeals sent by my health provider.”
What If I Don’t Hear Back?
Ignoring appeals is illegal. If your insurer doesn’t respond within the required timeline, you should file a complaint with your regulator—typically your state's Insurance Commissioner or the Department of Labor if you're on a self-funded plan.
Here's a breakdown of who to file a complaint with, depending on your plan type:
- Department of Labor (EBSA / ERISA): For self-funded employer plans
- State Departments of Insurance: For fully-insured employer plans, state or local government employers, and individual or exchange-purchased plans
- Centers for Medicare and Medicaid Services: For Medicare and Medicare Advantage plans
- State Medicaid Agencies: For Medicaid plans
- Office of Personnel Management : For federal employer plans

Denied your appeal? Don’t give up. Learn about your options for internal and external appeals, regulatory complaints, and legal action to fight for the care you need.
I know how frustrating it can be to receive another denial after you’ve already fought so hard. But I want to encourage you—this isn’t the end of the road. Many patients successfully win their second or even third appeal, and I’m here to help you get through this process. At Claimable, we’ve seen firsthand how persistence can pay off, and I want to make sure you have everything you need to keep moving forward.
Let’s walk through your options and how you can strengthen your next appeal.
My appeal was denied - can I file another appeal?
Yes! You have the right to multiple levels of appeal. These usually include internal reviews by your insurance company and external reviews by independent bodies. Your denial notice will explain how to re-appeal, including options for urgent cases.
How do I strengthen my next appeal?
Here’s what we’ve learned from analyzing successful appeals:
- Activate Influencers: Journalists, healthcare providers, or even industry leaders and politicians can help put pressure on insurers.
- Executive Outreach: Appeals directed to senior executives (like the CEO or medical officers) often get faster responses.
- Employer Outreach: If you’re in a self-funded plan, your employer’s leadership (like the CEO or CFO) is ultimately responsible for the plan.
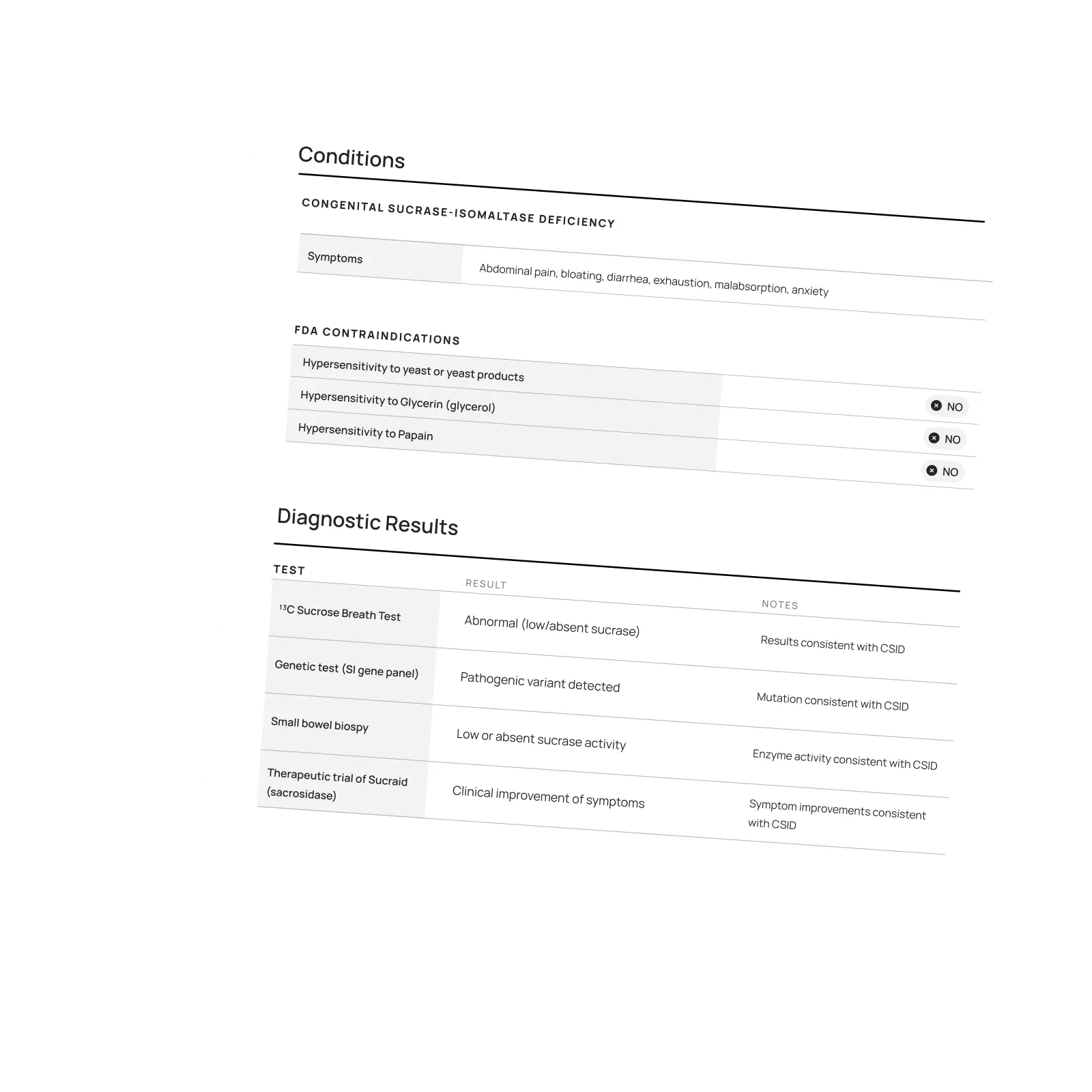
- Review Your Claim File: Look for mistakes or inconsistencies that can strengthen your appeal.
- Build Your Case: If the insurer took too long, used unqualified reviewers, or broke any rules, that can boost your chances.
- Legal Support: If your case is urgent or complex, consider reaching out to a legal expert.
What are the different levels of appeal options?
STEP 1
Internal Appeals
This is your first step—ask your insurance company to reconsider. You may need to appeal twice before moving to an external review. Be sure to submit any new evidence or arguments.
STEP 2
External Appeals
An independent board will review your case and make a decision, assigning a medical expert or review board. If they overturn the denial, your insurer must comply.
STEP 3
Regulatory Complaints
If your appeals aren’t successful, you can file a complaint with a regulatory agency, which may decide to investigate and intervene on your behalf.
STEP 4
Legal Action
If all else fails, legal action may be an option. Self-funded plans, Medicare, and federal employer plans usually go to federal court, while other plans often go to state court.
Appeal Options by Health Plan Type:
Self-Funded Employer Plans (most large insurers)
Appeal options:
1st: Internal Review
2nd: Internal Review*
3rd: External Review
4th: Regulator Complaint
5th: Legal Action
Relevant regulator:
Employee Benefits Security Administration (EBSA)
Fully-Insured Employer Plans
Appeal options:
1st: Internal Review
2nd: Internal Review*
3rd: External Review
4th: Regulator Complaint
5th: Legal Action
Relevant regulator:
State Insurance Commissioner (NAIC)
Individual / Exchange Plans
Appeal options:
1st: Internal Review
2nd: Internal Review*
3rd: Regulatory Complaint
Anytime: Legal Action
Relevant regulator:
State Insurance Commissioner (NAIC)
State & Local Government Employee Plans
Appeal options:
1st: Internal Review
2nd: Internal Review*
3rd: External Review
4th: Regulator Complaint
Anytime: Legal Action
Relevant regulator:
State Insurance Commissioner (NAIC)
Federal Employee Health Benefits
Appeal options:
1st: Internal Review
2nd: OPM Review
4th: MSPB Review*
5th: EEOC or OSC Complaint
Relevant regulator:
Office of Personnel Management (OPM)
Medicare & Medicare Advantage
Appeal options:
1st: Internal Review
2nd: External Review
3rd: OMHA/ALJ Hearing
4th: Appeal Council Review
5th: Judicial Review
Relevant regulator
Centers for Medicare & Medicaid Services (CMS)
Medicaid
Appeal options:
1st: Internal Review
2nd: Local Hearing*
3rd: State Hearing
4th: Office of Appeals*
5th: Legal Action
Relevant regulator:
State Medicaid Agency
* Optional or not always part of the process.
** See TRICARE and the Veterans Affairs for military or veteran related appeals.
Can Government Agencies Help?
Yes! Insurance plans are regulated by federal or state agencies that handle complaints and make sure insurers follow the rules. Here are some key regulators to know:
- Department of Labor (EBSA / ERISA): For self-funded employer plans
- State Departments of Insurance: For fully-insured employer plans, state or local government employers, and individual or exchange-purchased plans
- Centers for Medicare and Medicaid Services: For Medicare and Medicare Advantage plans
- State Medicaid Agencies: For Medicaid plans
- Office of Personnel Management : For federal employer plans
Do I Need Legal Help?
Claimable doesn’t provide legal advice, but if you’ve exhausted your appeals or face an urgent issue, legal support might help. Look for attorneys who specialize in health insurance denials—especially in cases involving bad faith or breach of contract.
Resources For Financial Help
If the costs are piling up, consider these resources:
- Patient Assistance Programs: Offered by pharmaceutical companies to provide free or discounted medications.
- Non-Profit Organizations: Groups like HealthWell Foundation, PAN Foundation or Good Days help cover treatment costs.
- Discounts, Coupons or Copay Cards: Pharmaceutical companies or third parties like GoodRx offer coupons, rebates, savings cards, free trial cards or free samples.
- Government Programs: Medicare Part D Extra Help or Medicaid offer financial aid.
- Debt Forgiveness: Programs like Undue Medical Debt or Dollar For help with medical debt relief.
Want to Learn More?
We highly recommend Marshall Allen’s book, Never Pay the First Bill: And Other Ways to Fight the Health Care System and Win, for more tips on navigating the healthcare system.
Featured stories
In the news
Download a winning sample appeal
Want to see what it takes to successfully overturn a health insurance denial? Download our sample appeal to learn how we build strong, evidence-based cases that get results.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Each month, I endure about eight major episodes, each one leaving me exhausted, unable to concentrate, and too unwell to take part in daily life.
The frequency and unpredictability of these symptoms have isolated me socially and limited my capacity to take part in activities most people take for granted.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!

One of our core principles is to help patients protect their rights and level the playing field with their insurance company. This includes rights to multiple appeals, fair reviews, decision rationale, exceptions when needed, and adequate network access, among others. For more, read our post on patients rights.
Claimable’s AI-powered platform analyzes millions of data points from clinical research, appeal precedents, policy details, and your personal medical story to generate a customized appeals in minutes. This personalized approach sets Claimable apart, combining proprietary and public data, advanced analysis and your unique circumstances to deliver fast, affordable, and successful results.
We currently support appeals for over 85 life-changing treatments. Denial reasons may vary from medical necessity to out of network, and we even cover special situation like appealing plans that won’t count your copay assistance towards your deductible (hint: those policies were banned at the federal level in 2023). That said, we are rapidly growing our list of supported conditions, treatments and reasons. You can quickly check eligibility and ask to be notified when your interest becomes available. It helps us know where to focus next 🙂
We think about appeal times in a few ways. First, many professional advocates and experienced patients spend 15, 30 or even 100 hours building an appeal–but with Claimable, this takes minutes. We automate the process of analyzing, researching, strategizing and wordsmithing appeals. Next, there is the process of figuring out where you will send it (hint: expand your reach beyond appeal departments), then printing, mailing and/or faxing your submission. We handle that, too. Finally, there is the time it takes to get a decision. We request urgent reviews when appropriate, and typically receive standard appeal decisions within a couple weeks.
Review periods are mandated by applicable laws, from 72 hours for urgent, 7 days for experimental, 30 days for upcoming and 60 days for received services. Our goal is to get a response as fast as possible, since most of our clients are experiencing long care delays or extreme pain and suffering.
Claims are denied for a variety of reasons, many of which blur definitions. We focus on helping people challenge denials by proving care is needed and meets clinical standards, in addition to addressing specific issues like experimental treatments, network adequacy, formulary or site of care preference exceptions. We don't support denials for administrative errors or missing information, as we think those are best handled by simply resubmitting the claim in partnership with your provider. That said, many of our most rewarding successes have been cases previously though 'unwinnable', with providers and patients who fought tirelessly for months without appropriate response or resolution.
A denial letter is a formal notice from your insurance company explaining why a claim was denied and how you can appeal the decision. Sometimes the notice is included within an Explanation of Benefits. It is a legal requirements; if you didn’t receive one, contact your insurance company.
A letter of medical necessity is a statement from your doctor justifying why a specific treatment is critical to your care and/or urgently needed. You can attach it to your patient appeal to strengthen your case, especially if you are requesting an urgent appeal or need to skip standard ‘step therapy’ requirements. That said, we don’t require them and are often successful without them.
A claim file contains all the documents and communications your health plan used to decide whether to approve or deny your claim. Most health plans are legally required to share this information upon request. According to a ProPublica investigation, reviewing your claim file can help expose mistakes or misconduct by your health plan, which can make your appeal stronger.
Your insurer is required by law to give you written information about how to appeal, including the name of the company that reviewed your claim and where to send your appeal. Your health insurer may work with other companies, such as Pharmacy Benefit Managers (PBMs), Third-Party Administrators (TPAs), or Specialty Pharmacies, to manage your claims. These companies might be responsible for denying your claim and handling the appeal process on behalf of your insurer.
If you don't win your first appeal– don't give up! Many people are successful on their 2nd, 3rd or even 4th try, and future appeals are reviewed by independent entities. That said, we wrote a whole guide to understanding your options, including escalating your appeal and seeking other assistance for covering costs, forgiving debt or even seeking legal or regulatory support.
While both denial rates and appeal success rates vary widely by the type of health plan, state, and insurance company, studies have shown more than 50% of people win their appeal–and we apply strategies to boost your chances of success. Claimable has an 80% appeal success rate. The biggest denial challenge is that most people never appeal–allowing unjust denials to control their healthcare options because they are unaware of their rights or lack the support needed to fight back. No one needs to fight alone–Claimable is here to help. We know first hand that many denials are based on errors, inconsistencies or auto-decisions, and have proven strategies for fighting back against this injustice.
Let’s get you covered.