Why You Should Appeal Your Insurance Denial Yourself — Not Just Leave It to Your Doctor

When your insurance denies coverage for something your doctor says you need, it can feel like hitting a wall. The treatment is medically necessary. Your provider agrees. And somehow, your insurer still says “no.”
At that point, most people do the same thing: they call their doctor’s office and ask them to help. That makes sense – most patients haven’t had to appeal an insurance decision before, and assume that since the prescription came from their doctor, so should the appeal to cover it.
But here’s what most people don’t know: health insurance appeals aren’t just medical arguments. They’re regulatory, contractual, and strategic. They require paperwork, persistence, and the ability to challenge a policy – not just explain a diagnosis.
Saying the quiet part out loud: your doctor’s appeal isn’t always enough. Sometimes, it’s not even the best place to start. That’s why if you want the best shot at getting coverage approved, you should appeal it yourself.
What’s the difference between my appeal and one that comes from my doctor?
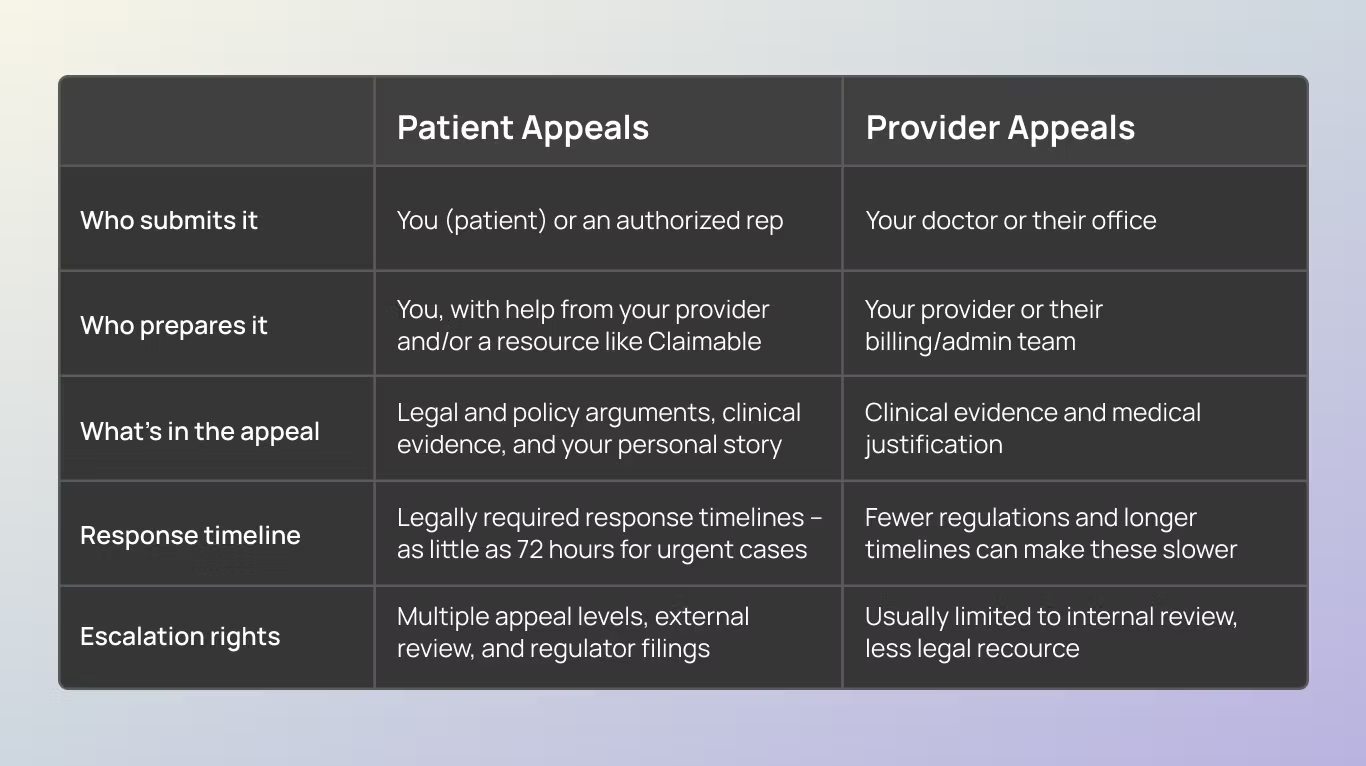
When your insurer denies a medication, treatment, or service, there are two types of appeals that can be submitted:
- A provider appeal is when your doctor or their billing team contacts your insurer to argue that the treatment is medically necessary. These usually happen through the insurer’s internal system and often involve submitting clinical documentation.
- A patient appeal is when you, the person covered by the plan, formally challenge the denial. This taps into patient and consumer protections, and gives you access to additional tools, like independent reviews and mandated timelines and processes.
They may sound similar, but they vary. How are these types of appeals different?
Now you can see some of the strengths that come from choosing to appeal yourself, as a patient – but it might still seem scary to take on. Apprehension about appeals isn’t an accident – insurers have spent years trying to make this seem hard, so people don’t do it.
Common misconceptions about insurance appeals – and what they get wrong.
If you’ve never appealed an insurance denial before, you’re not alone (and you’re not behind). Most people don’t learn how this works until they have to.
This is often made harder by the assumptions people make about appeals. Here’s three of the most common misconceptions—and the truth about what actually works when you’re fighting a denial.
Misconception #1: “My doctor will take care of it.”
We hear this all the time. You get denied, and your first call is to your doctor to ask what to do. After all, they prescribed the treatment – surely it’s up to them to explain why you need it covered, right?
Why this doesn’t work:
Your doctor can support an appeal, but they’re not insurance policy experts – and more importantly, they’re not the one whose plan is in question here. Their top priority is to care for their patients, and they have limited options and resources to address the rising denial volume.
The reality:
You, the patient, hold the contract. The job of an appeal is to prove a denied treatment or service was contractually obligated to be paid for. This is equal parts a patient and consumer protection issue.
Misconception #2: “I don’t know how to do this — I’ll mess it up.”
It makes sense to feel this way – the healthcare system is overwhelming, and insurance is confusing on purpose. They want you to give up. That means that if you’ve never appealed before, it can feel like you’re not qualified to try.
Why this doesn’t work:
Assuming you’re not capable leads to inaction while you search for someone else to do it. Lawyers are expensive and don’t take many cases. Doctors don’t have the time, resources or rights to escalate appeals. And every time an unjust denial goes unchallenged, insurers are emboldened to deny more medically necessary care.
The reality:
Not long ago, it felt impossible to make this case on your own. Not anymore. With tools like Claimable, all you have to do is share your story and answer a few easy, guided questions. Then, we’ll pull all of the right laws, policies, and studies to make you the strongest appeal.
Misconception #3: “Its pointless — If they denied me, it must not be covered.”
This is what insurance companies want you to believe. That a denial is final, that you’re out of options, and that fighting back is too complicated or hopeless to be worth it.
Why this doesn’t work:
It causes people to give up on treatment they need, or to pay out-of-pocket for something their insurance might have covered – if only they had pushed back.
The reality:
Insurance companies deny coverage in error all the time – either due to mistakes or misconduct. Appealing is a built-in protection from a broken system. In fact, more than half of denials are overturned on appeal – and you have the power to take them on.
Why you should lead your own appeal
The best person to advocate for your care is you. Here’s why:
You hold the contract (and the legal rights that go with it)
Your doctor is there to care for you — but you’re the one who has a legal agreement with your insurance company. That gives you rights your doctor doesn’t have on their own, including state and federal protections.
When you appeal directly, you can:
- Trigger faster, legally mandated response times (like 72 hours for urgent cases)
- Escalate to external reviewers or regulatory agencies – including the ability to file complaints with your state’s insurance board
- Demand a full, fair review based on your policy’s language
You can move faster
When providers appeal, the paperwork often gets routed through internal insurer systems that are slow, opaque, and hard to track. Appeals can get stuck in “processing” or lost altogether.
When you appeal yourself, you’re in control. You don’t have to wait for office staff to call the insurer back or follow up on a fax. You set the pace – and you can hold your insurer accountable for timely responses.
You can make a stronger, more complete case.
Provider appeals are almost always focused only on clinical information. But winning an appeal often requires:
- Legal or regulatory arguments
- Citing FDA standards or policy precedent
- Personal impact statements about how the denial is affecting your life
Your doctor isn’t trained in insurance law. And they shouldn’t have to be. By appealing yourself — especially with help from a tool like Claimable — you can bring all these elements together into a comprehensive case that’s much harder to ignore.
You care the most – and in your appeal, that shows
Your doctor has hundreds of patients, dozens of responsibilities, and limited time. Appeals are just one more administrative burden in a broken system.
But for you, this appeal matters. It’s your treatment, your time, your health. That motivation — paired with the right tools — is what makes you the most effective person to lead the charge.
Why doctors don’t always win appeals (and that’s ok)
When you bring a denial to your doctor, they do what they can. A good provider is invested in your care, and they want to help get you the treatment they’ve prescribed. But the truth is: most provider-led appeals are brief, clinical, and limited in how far they can go.
Why? Doctors have no power over the insurance company. They don’t hold an insurance contract (like you do). And the system is set up to make it all too easy for the insurer just to say no all over again.
Here’s how provider appeals typically go:
- First, they write a letter of medical necessity and send it over.
- Once insurance denies it again, your provider has a “peer-to-peer review” with a doctor who works for the insurance company. The reality? The job of the peer reviewer is to explain to your doctor why the insurer isn’t going to pay for it.
- And that might be it – they’ve reached the end of the road on this appeal.
That’s not their failure – it’s just a reflection of the system. Doctors aren’t trained or resourced to fight complex coverage decisions. That’s not what they went to med school for. They’re here to take care of you. The rest is up to you – and tools like Claimable.
How to work with your doctor – while staying in the drivers’ seat on your care
Appealing yourself doesn’t mean doing everything alone. Think of it like this: you’re the quarterback, and your provider is your key teammate.
When you get denied, here’s how to work with your doctor on your appeal.
- Loop them in: Let their office know that your medication or service was denied, and that you plan to submit your own appeal. Most will be supportive — and sometimes relieved — that you’re taking the lead. Try this:
- “I’m planning to appeal my denial directly, since I can escalate it beyond internal review. Would you be willing to support the appeal with a letter or documentation showing this treatment is medically necessary?”
- Ask for what they do best: Medical support. You don’t need them to write a legal brief – just a solid medical explanation. Request:
- A Letter of Medical Necessity (try our LOMN template to make it easy!)
- Diagnosis codes and chart notes\
- Any history of treatments that didn’t work
- Keep communication clear and focused. No need to forward your entire appeal draft. Instead:
- Summarize what you’re submitting
- Make 1–2 specific asks
- Respect their time — they’ll appreciate it
- Follow up and share your success: Let your provider know the outcome of the appeal. It helps close the loop and might even help future patients.
The easiest, most effective way to do your appeal
By now, we hope you see the value in taking charge of your appeal – and your care – directly. But researching all of the laws, policies, and . Luckily, you don’t need to be an insurance expert to write a winning appeal. That’s exactly what we built Claimable to do.
Here’s how it works:
- You answer a short set of questions about your medical and personal history
- You provide key documents, like your doctor’s letter of medical necessity
- We incorporate legal precedent, policy, and clinical standards
- We create a strong, customized appeal with the best arguments
- You approve – and we automatically sent it to your insurer and other key recipients
It’s that easy. In minutes – not days – you can build a case and fight back against your denial. And win.
The bottom line: You’re the best person to fight for your care
Your doctor is here to care for you. Your insurer is here to protect their business. And you? You’re the one who has the most to gain – or lose – from this decision.
Insurance companies count on confusion. On delays. On patients giving up. But you don’t have to play by those rules.
By appealing directly – and using every right the law gives you – you give yourself the best chance at getting the care you need. With your doctor on your side and Claimable in your corner, you’re not just filing an appeal. You’re creating a case that’s built to win.
You have the right. You have the tools. You’ve got this.
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!