Resources
Latest Posts
At Claimable, we’re dedicated to empowering patients to fight for the care that they deserve. That’s why, as of today, we’re officially supporting free second-level appeals for CVS Caremark Zepbound forced-switch denials — so you can be confident your case receives a full, fair, and individualized review.
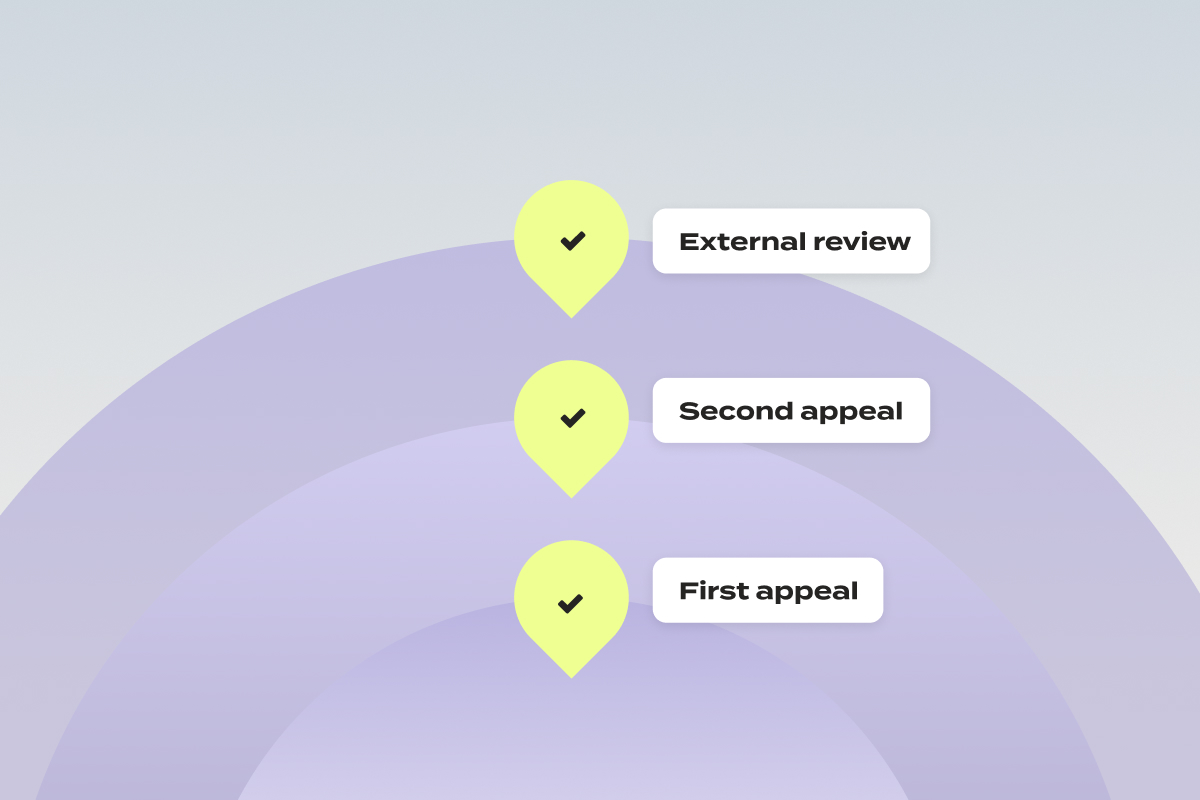
First, What’s A Second-Level Appeal?
When you submit an appeal as a patient and it’s denied, it isn’t the end. You have the right to request a second-level appeal, which often involves review by a different department or an independent third party. Put simply? It’s another chance to have your case heard, and have your denial overturned.
Why We’re Escalating to Second-Level Appeals
Over the past weeks, we’ve had an influx of patients file appeals for Zepbound coverage with CVS Caremark. Unfortunately, we’ve begun to see responses to those appeals come back as form-letter denials – ignoring not only your unique health history, doctor’s notes, and plan details, but also state and federal laws. Federal rules are clear: every appeal must receive an individualized review. The copy paste answers we’re seeing? They’re not that.
In order to make sure that each of these appeals get the full and fair review they’re entitled to, it’s time to escalate it to the next level:
- Internal vs. External Reviews
- Internal appeal: Your denial is reviewed by CVS Caremark or your insurer. Yes, the same company that issued the denial – though federal law requires that the review be conducted by someone who wasn’t involved in the original decision.
- External appeal: Also called an external review or, in some states, an Independent Medical Review (IMR). This is conducted by a licensed medical professional or organization not affiliated with your insurance provider, using objective, evidence-based criteria. External decisions are binding on the insurer, but you may still have the right to pursue legal action if the outcome is unfavorable.
For forced-switch denials of Zepbound, we pursue the external review – most likely to secure the coverage you need — free of charge.
What to Expect If Your First Zepbound Appeal Is Denied
- You Report the Denial
Once you get the notification that your appeal has been denied, simply log into your Claimable account to report the outcome – or email us at support@getclaimable.com - You Consent To Escalation
We’ll confirm you’d like to continue to escalate to a second-level appeal. At this point, you’ll upload your appeal denial letter. - We Build Your Strongest Case
Once you consent, we’ll generate your second-level appeal package. This includes a newly drafted appeal letter with an expert legal opinion and your prior appeal materials. - You Review & Submit
We’ll notify you when your second-level appeal is ready for review. You’ll confirm where to send (fax/mail) your appeal, then click “Submit” once everything looks right. - We Send – Expedited
Claimable will fax and mail your appeal to both CVS and the independent reviewer.
Because all Zepbound forced-switch appeals involve ongoing treatment for a serious condition, your case will be marked urgent – requesting an expedited external review. This means that in most cases, the reviewer must issue a decision within 72 hours, though some may take longer.- You Get Notified
You’ll be notified of the outcome via portal message, email, or phone, as well as receiving a mailed copy of the decision.
If it’s approved? The decision is binding – and CVS must cover your Zepbound.
Key Questions – Answered
What is a second-level appeal?
It’s your right to request another review when your first appeal is denied—either internally by the insurer or externally by an independent reviewer. We choose the path most likely to win for you.
Why is Claimable offering free 2nd-level appeals?
With these early Zepbound appeals, we’ve seen a clear pattern of “cookie-cutter” denials that violate the full-fair-and-individualized-review requirement. To level the playing field, we’re offering these escalations free of charge to demand unbiased consideration.
Keep in mind, this only applies if you submitted your first-level appeal through Claimable. If you've appealed a different way and think you might need a second-level appeal, feel free to email us for help navigating the process.
What’s included in my Claimable second-level appeal?
A freshly drafted appeal letter with expert legal commentary, your first appeal materials, and previous denial letters—packaged to maximize your chance of success.
Is there any cost to second level appeals?
Nope – this service is completely free for CVS Caremark Zepbound forced-switch cases. Claimable’s appeal strategy is customized for each insurer and medication—and in these cases, supporting a second-level appeal is part of our core approach to winning.
What do I need to submit a second-level appeal?
You’ll need your appeal denial letter to confirm the instructions for submitting a second-level appeal, including where to send it and whether any forms are required.
If you’ve received your claim file and designated record set since initially submitting, we recommend uploading them when prompted (after you review your second-level appeal draft).
How do I track my appeal’s status?
If you haven’t heard back within 72 hours, call the number on your insurance card. Otherwise, we’ll notify you as soon as the reviewer issues a decision.
Do I have to redo the appeal questionnaire?
Never. All your first-level answers and uploads carry over automatically.
We know the appeals process can feel confusing and overwhelming. That’s why we built Claimable — to guide you every step of the way. With our new second-level appeal support, you can rest assured that we’ll fight tirelessly to get you the coverage you deserve.
Questions? We’re here for you. Reach out to support anytime.

The past few years have brought major progress in how we prevent and manage migraine. CGRP-targeting medications like Aimovig, Emgality, Vyepti, Nurtec ODT, and Qulipta represent a shift in both the science and strategy of treating this condition.
They're often better tolerated and more effective than older medications, and they allow for more personalized care, whether that means a daily pill, a monthly injection, or a quarterly infusion.
But while the science has advanced, insurance coverage hasn't kept up. Patients are still being denied access to these medications due to outdated policies, arbitrary formulary changes, and one-size-fits-all coverage rules. At Claimable, we're working with patients, providers, and advocacy partners to challenge these barriers—and win.
If you're facing a denied claim for a migraine medication, read on to understand the tactics insurance companies take to limit access to these treatments – and what you can do to get covered.
Understanding the migraine treatment landscape
As a migraine sufferer, I know that migraines are more than a bad headache. It's a disabling neurological disease that affects over 40 million people in the U.S. and is a leading cause of missed work and reduced quality of life.
CGRP (calcitonin gene-related peptide) medications have transformed our ability to treat and prevent migraine. Unlike older medications developed for other conditions (like epilepsy or depression), CGRP drugs are designed specifically for migraine. They target the biological mechanisms believed to drive attacks, offering relief with fewer side effects.
Why migraine coverage is so challenging
Even though these medications are FDA-approved and supported by professional guidelines, insurance plans often:
- Require you to fail older, less effective drugs first
- Only cover one CGRP drug despite clinical differences
- Force patients to switch medications mid-year due to rebate deals
- Approve treatment only temporarily, requiring re-authorization every few months
- Use vague or bureaucratic reasons to deny access altogether
This system doesn't reflect the complexity of migraine or the individual needs of patients. It reflects cost-saving tactics that delay care.
Common migraine insurance denial reasons – and how we fight them
Step Therapy Requirements
What it is: Insurance insists you try and fail older medications (like triptans, topiramate or amitriptyline) before approving CGRP drugs.
Why it's wrong: These older medications often come with tough side effects and weren't designed for migraine. The American Headache Society supports CGRP drugs as a first-line option.
How we fight it: We submit detailed appeals outlining your treatment history, side effects from older meds, and professional guidelines that justify bypassing step therapy.
Formulary exclusions
What it is: Only one CGRP medication is covered. All others are denied.
Why it's wrong: CGRP drugs aren't interchangeable. A daily pill may work better for one person than a monthly injection. Side effects and effectiveness vary.
How we fight it: We explain the medical rationale for your chosen medication, using provider notes and evidence that shows why it's not just a preference—it's a necessity.
Mid-Year medication switching
What it is: Your plan changes coverage mid-year due to PBM rebate deals, forcing you to switch medications from a medication you're stable on to what they prefer.
Why it's wrong: Migraine treatment relies on consistency. Switching meds can cause rebound attacks and destabilize your care.
How we fight it: We focus on treatment stability and cite ERISA protections (if applicable) to challenge the fairness of mid-year changes.
Short-term or conditional approvals
What it is: You get approved for 30 or 60 days at a time, with constant re-authorization requirements.
Why it's wrong: Migraine is chronic. Short-term approvals create anxiety, disrupt care, and burden providers.
How we fight it: We argue for long-term approval based on your condition and medication response, using both legal framing and clinical support.
"Not medically necessary" determinations
What it is: Your insurer denies a medication without a clear reason, claiming it's not necessary.
Why it's wrong: This ignores your provider's judgment and contradicts clinical guidelines.
How we fight it: We present peer-reviewed studies, your provider's rationale, and documentation showing how the treatment improves your quality of life.
Administrative or documentation barriers
What it is: Missing forms, technicalities, or unclear instructions result in denials.
Why it's wrong: The insurer is making medical decisions by burying you in paperwork. Most people give up and concede to insurance demands. It's generally understood that patients who accept non-medical switches have adverse side effects and poorer outcomes.
How we fight it: We ensure everything is submitted cleanly and correctly, with language that anticipates common administrative objections.
How Claimable builds strong migraine appeals
As a patient, you have the right to challenge these denied claims. Insurers are required to comply with state and federal laws – which often require their denial rationale to be based on medical necessity, FDA standards, and other clinical, legal, and policy standards.
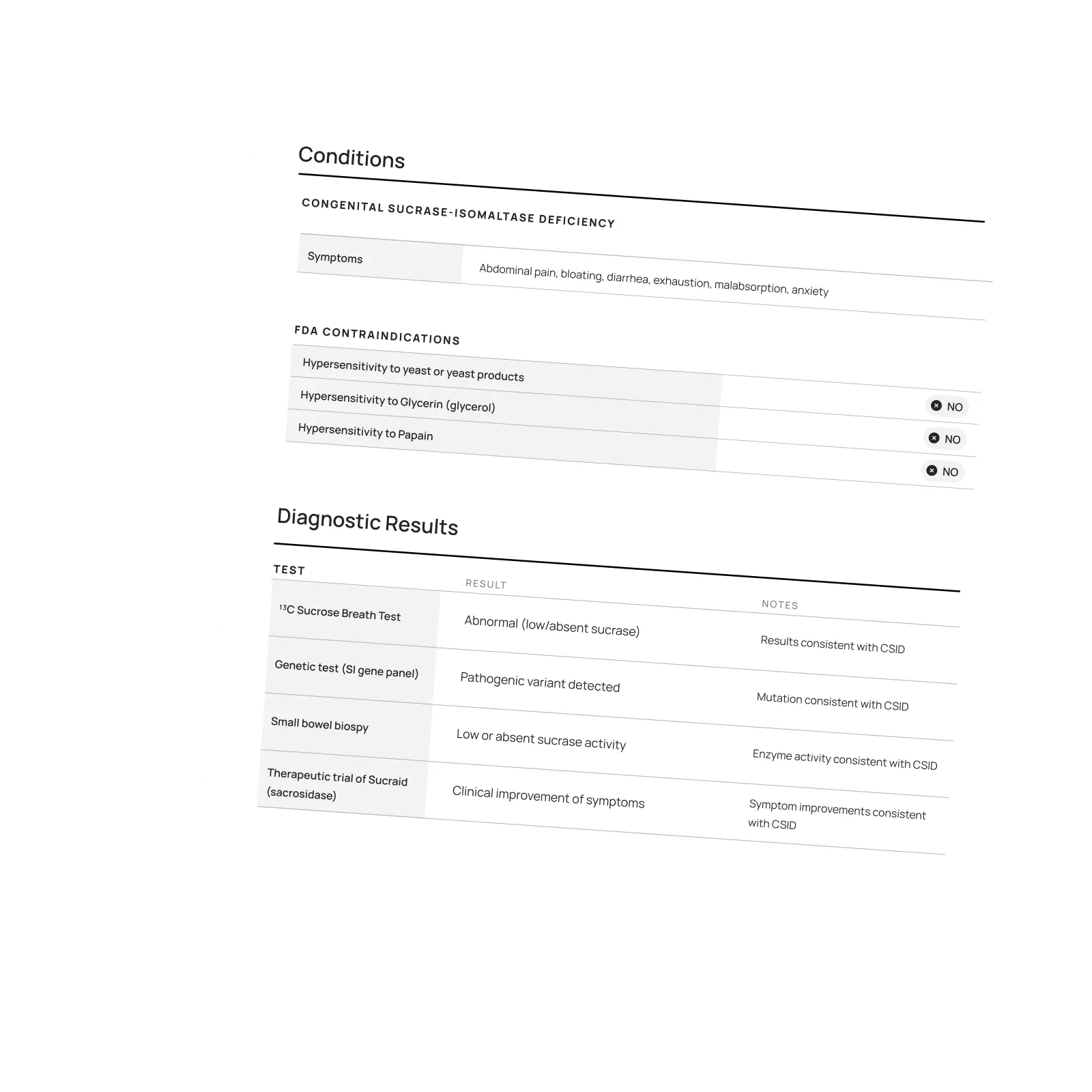
That means a strong appeal should include clinical evidence, legal standards, and policy compliance to hold insurance accountable to deliver your care and coverage. At Claimable, we use a multi-layered approach:
- Personal narrative: We capture your history, prior treatments, and how migraine affects your life. In particular this could be how you're not able to enjoy your hobbies or do basic things like drive safely at night. We hear of patients becoming socially isolated.
- Clinical evidence: We include the latest guidelines, studies, and medication-specific data. This includes the guidance from the American Headache Society, and other peer-reviewed studies and randomized controlled trials proving these medications are right for you.
- Legal leverage: We reference plan terms, medical necessity requirements, and ERISA protections. This helps reinforce your rights to have a full and fair review of your care. An insurance doctor who has never met you shouldn't get to make the call.
- Collaborative advocacy: Your primary care doctor or neurologist can refer you for an appeal if they have a denial, or you can simply add their letter of medical necessity to your appeal to increase its strength.
Why this work matters – unlocking migraine coverage
The medications now available can change lives. But they only work if you can access and stay on them. No one should be forced to suffer just because their insurer hasn't updated its playbook.
At Claimable, we don't just file paperwork. We build appeals that reflect who you are, what you've been through, and why your treatment plan matters. If your migraine medication has been denied, disrupted, or downgraded, we'll help you fight back—with precision, evidence, and persistence. Your journey matters to us.
Facing an insurance denial for Aimovig, Emgality, Nurtec or other migraine medication?
We're here to help. Let's make the system work for you—not against you.
Get started on your migraine appeal today.
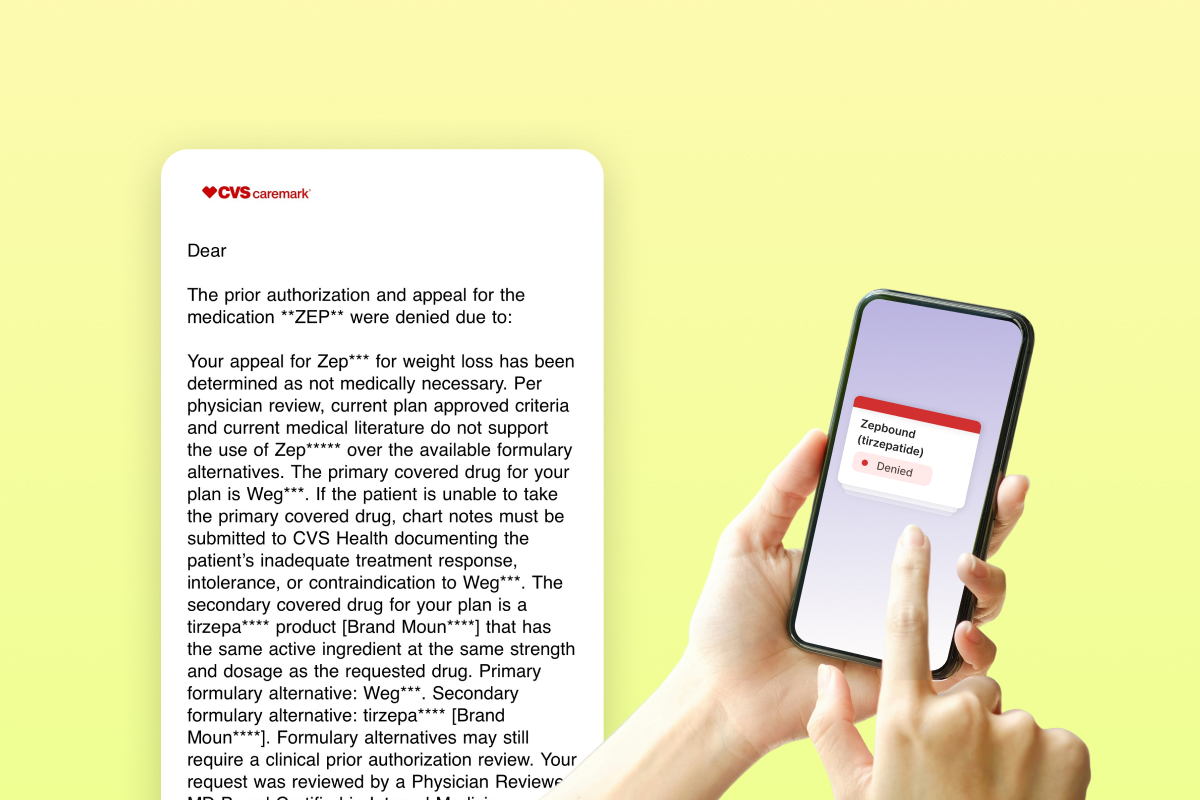
The first responses to Zepbound appeals for the CVS Caremark forced switch have started to come in. Claimable COO Alicia Graham breaks down what's in these new denial letters, and what that means next.
If you've gotten one of these letters, know that we're going to keep fighting it. We don't believe this rationale is based on medical necessity, nor that it will hold up to a secondary review. We're actively escalating these appeals, because we believe that you will win.
This thing is getting more ridiculous by the day. As we start to see responses come back to CVS Caremark, I wanted to share what we've been seeing – because frankly, a lot of what they've said so far is vague, misleading and even straight up false. I don't believe these denials are in compliance with the plan policy, applicable laws, or clinical standards of care at all, and we're going to break down why that Is.
This is my take on exactly what's in these denial letters, what it actually means, and what you can do if you got one. I know how confusing this is, and I hope this can help anyone navigating it.
The one size fits all "coverage request was not approved" denial letter

First of all, this is the language we're seeing in almost all of these letters – just copy-pasted for everyone. By law, each appeal needs to be reviewed by a qualified human performing a full and fair review of specific case facts… so straight off the bat, it doesn't look like they're doing that.
"Your appeal for Zepbound has been determined as not medically necessary"
They say that current medical literature doesn't support the use of Zepbound over the available formulary alternatives. Except it does (here's the head-to-head study we've been including in our appeals). They conveniently don't include the studies they use to make their decision, which they're supposed to do… so we have no idea why they ignored it and what they are using instead.
Plus, they're saying Zepbound isn't medically necessary, but Wegovy and Mounjaro are?! I don't understand how that argument could ever stand up in a court. Wegovy is indicated for the same treatment with same coverage criteria, and Mounjaro... isn't even indicated for weight loss.
"The primary covered drug for your plan is Wegovy"
"If the patient is unable to take the primary covered drug, chart notes must be submitted to CVS Health". What they're saying here is if you fail Wegovy, you could get back on Zepbound. This is step therapy, but in lots of states there are laws against this. If you live in New York, for example, they cannot require you to have previously failed Wegovy – but we're seeing them do it anyway.
If you live in New York and got this, you should definitely fight it.
"The secondary covered drug for your plan is a tirzepatide product [Brand Mounjaro]"
This is a curveball – not what we expected to see. Yes, Mounjaro is a tirzepatide like Zepbound, but per the FDA it is only approved for type 2 diabetes.
If you and your doctor agree on you taking Mounjaro off-label, great! That's completely up to you and what's best for your care. But for your insurer to try to force you onto an off-label indication? Unethical, clinically absurd, and probably illegal.
But even more importantly this smells like a trap to me.
The trap: "Formulary alternatives may still require a clinical prior authorization"
They're saying that Mounjaro may still require a PA. We've seen this before, so I want patients and providers to clearly understand the risk of going down this path.
The PA form states you do not qualify for Mounjaro unless you have type 2 diabetes, so the minute they ask for a PA your Mounjaro coverage will be gone. Even if they approve you without a PA today, at any time they can come back ask for it which will kick you off.
This has happened to several patients we've worked with who took Mounjaro for months and then were told they don't qualify. They can force you off at any time because the criteria for Mounjaro is different.
The trap within the trap: The 180 day appeal window
I think a big part of them trying to lure you into doing Wegovy or Mounjaro is that by law, you only have 180 days to appeal your Zepbound denial. Hypothetically they could cover Mounjaro for those 180 days, and then on day 181 when that window expires and you've lost your right to fight for Zepbound, revoke your approval for Mounjaro – leaving you with nothing.
Even if you want to try Wegovy or Mounjaro, I would keep going on your Zepbound appeal at the same time. If you win a Zepbound appeal, they can't just take it away.
Robocalls, app messages, and other nonsense
Legally, they have to send you a formal letter with details, full appeal rights, and more. But instead, they're sending these mini-messages ahead of time and telling you to wait for the letter.
Why? Because not having all the info makes your response weaker and slows things down. Make sure you request your full claim file, formal denial letter, drug policy and all other decision documents. You're legally entitled to them.
The bottom line: You don't have to let them win
The TLDR; these denials don't pass my smell test for compliance with the plan policy, applicable laws, or clinical standards of care. I don't think these will hold up in external review, courts, or with regulators. So I say keep fighting.
If you got one of these, first request all the documents. Then, escalate it. In your denial letter there will be a number/address for the external reviewer to send it to. **You have the right for an external review and I think that if you do you will win.
At my company this is exactly what we're doing. We're creating secondary appeals that address every single piece of BS in these letters and escalating them to reviewers and regulators. Because PBMs and insurers are watching this – and the last thing I want is to show them that pulling stuff like this is ok. It's not, and we're going to fight it. And win.
– Alicia
PS – if you only have the "a change is coming on July 1" letter
I've seen a lot of people try to appeal using these letters – this will not work. This letter is not a denial of coverage for Zepbound. All this tells you that they will deny it if coverage is requested after July 1, but you can't appeal based on this.
If you've only gotten this letter and want to try to stay on Zepbound, you need to get denied first. That means:
- Your provider needs to submit a new prior authorization request for Zepbound (form here)
- It's best to do this with a LOMN attached (template here, Lilly has one also)
- You wait until that prior authorization gets denied
- Then you can appeal
Featured stories
In the news
Download a winning sample appeal
Want to see what it takes to successfully overturn a health insurance denial? Download our sample appeal to learn how we build strong, evidence-based cases that get results.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Each month, I endure about eight major episodes, each one leaving me exhausted, unable to concentrate, and too unwell to take part in daily life.
The frequency and unpredictability of these symptoms have isolated me socially and limited my capacity to take part in activities most people take for granted.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!

One of our core principles is to help patients protect their rights and level the playing field with their insurance company. This includes rights to multiple appeals, fair reviews, decision rationale, exceptions when needed, and adequate network access, among others. For more, read our post on patients rights.
Claimable’s AI-powered platform analyzes millions of data points from clinical research, appeal precedents, policy details, and your personal medical story to generate a customized appeals in minutes. This personalized approach sets Claimable apart, combining proprietary and public data, advanced analysis and your unique circumstances to deliver fast, affordable, and successful results.
We currently support appeals for over 85 life-changing treatments. Denial reasons may vary from medical necessity to out of network, and we even cover special situation like appealing plans that won’t count your copay assistance towards your deductible (hint: those policies were banned at the federal level in 2023). That said, we are rapidly growing our list of supported conditions, treatments and reasons. You can quickly check eligibility and ask to be notified when your interest becomes available. It helps us know where to focus next 🙂
We think about appeal times in a few ways. First, many professional advocates and experienced patients spend 15, 30 or even 100 hours building an appeal–but with Claimable, this takes minutes. We automate the process of analyzing, researching, strategizing and wordsmithing appeals. Next, there is the process of figuring out where you will send it (hint: expand your reach beyond appeal departments), then printing, mailing and/or faxing your submission. We handle that, too. Finally, there is the time it takes to get a decision. We request urgent reviews when appropriate, and typically receive standard appeal decisions within a couple weeks.
Review periods are mandated by applicable laws, from 72 hours for urgent, 7 days for experimental, 30 days for upcoming and 60 days for received services. Our goal is to get a response as fast as possible, since most of our clients are experiencing long care delays or extreme pain and suffering.
Claims are denied for a variety of reasons, many of which blur definitions. We focus on helping people challenge denials by proving care is needed and meets clinical standards, in addition to addressing specific issues like experimental treatments, network adequacy, formulary or site of care preference exceptions. We don't support denials for administrative errors or missing information, as we think those are best handled by simply resubmitting the claim in partnership with your provider. That said, many of our most rewarding successes have been cases previously though 'unwinnable', with providers and patients who fought tirelessly for months without appropriate response or resolution.
A denial letter is a formal notice from your insurance company explaining why a claim was denied and how you can appeal the decision. Sometimes the notice is included within an Explanation of Benefits. It is a legal requirements; if you didn’t receive one, contact your insurance company.
A letter of medical necessity is a statement from your doctor justifying why a specific treatment is critical to your care and/or urgently needed. You can attach it to your patient appeal to strengthen your case, especially if you are requesting an urgent appeal or need to skip standard ‘step therapy’ requirements. That said, we don’t require them and are often successful without them.
A claim file contains all the documents and communications your health plan used to decide whether to approve or deny your claim. Most health plans are legally required to share this information upon request. According to a ProPublica investigation, reviewing your claim file can help expose mistakes or misconduct by your health plan, which can make your appeal stronger.
Your insurer is required by law to give you written information about how to appeal, including the name of the company that reviewed your claim and where to send your appeal. Your health insurer may work with other companies, such as Pharmacy Benefit Managers (PBMs), Third-Party Administrators (TPAs), or Specialty Pharmacies, to manage your claims. These companies might be responsible for denying your claim and handling the appeal process on behalf of your insurer.
If you don't win your first appeal– don't give up! Many people are successful on their 2nd, 3rd or even 4th try, and future appeals are reviewed by independent entities. That said, we wrote a whole guide to understanding your options, including escalating your appeal and seeking other assistance for covering costs, forgiving debt or even seeking legal or regulatory support.
While both denial rates and appeal success rates vary widely by the type of health plan, state, and insurance company, studies have shown more than 50% of people win their appeal–and we apply strategies to boost your chances of success. Claimable has an 80% appeal success rate. The biggest denial challenge is that most people never appeal–allowing unjust denials to control their healthcare options because they are unaware of their rights or lack the support needed to fight back. No one needs to fight alone–Claimable is here to help. We know first hand that many denials are based on errors, inconsistencies or auto-decisions, and have proven strategies for fighting back against this injustice.
Let’s get you covered.