Resources
Latest Posts
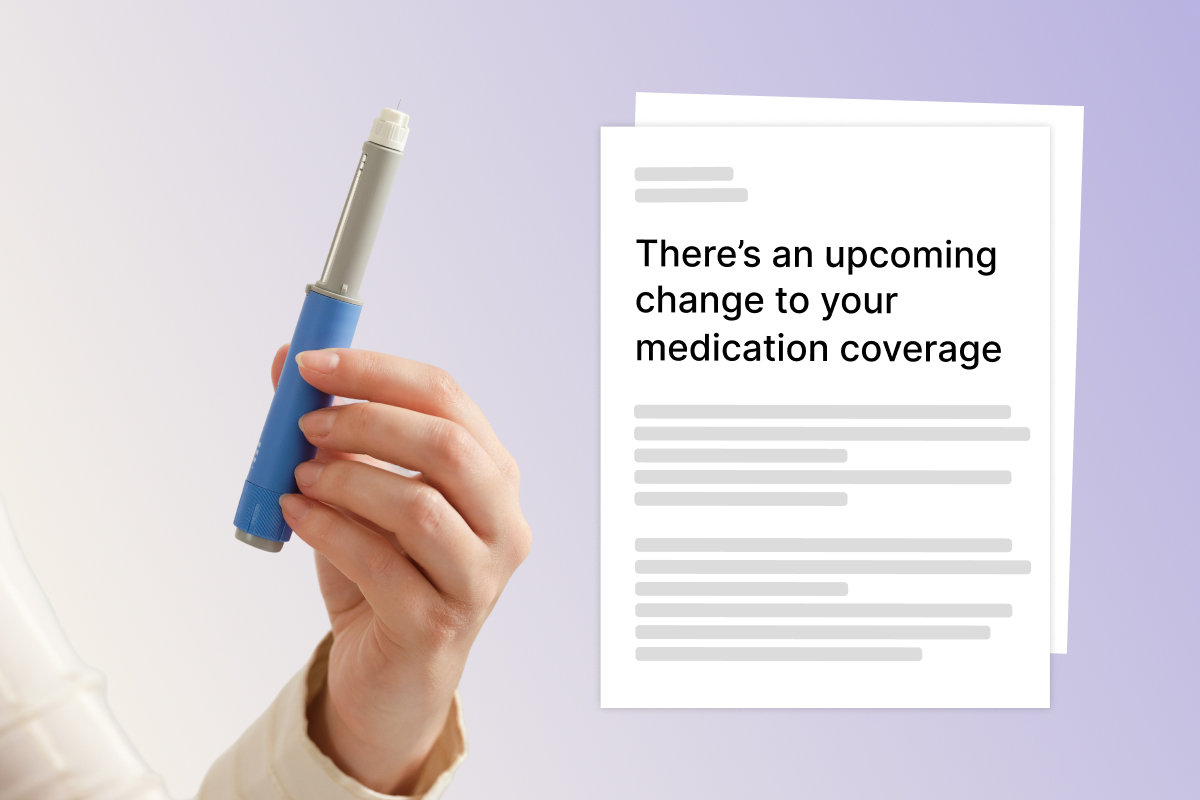
December 2025 update: This article was originally written in summer 2025 when CVS Caremark notified patients about a switch from Zepbound to Wegovy. Now, as plans renew for 2026, many people are receiving similar updates – Zepbound will no longer be on their formulary in the New Year. The good news? You can still submit a formulary request to keep coverage for Zepbound. Learn more about past formulary changes in this article, check out more on our Zepbound appeals here, or get started today.
Starting July 1, 2025, CVS Caremark will stop covering Zepbound – even if it's been working for you. Thousands of patients with conditions like obesity, obstructive sleep apnea, and other conditions are being notified that they must switch to Wegovy to stay covered.
If you received a letter saying your coverage is changing, you're not alone. And you have options. What's happening here is called a "formulary change", and while it may seem final, you can appeal – and win.
At Claimable, we help people fight insurance denials every day – which means this isn't our first forced switch, and it won't be our last. Read on for our guide on what you need to know, why it matters, and exactly how to push back to stay on the medication that's working for you.
Quick Summary: What you need to know
- CVS Caremark is removing Zepbound from its formulary starting July 1, 2025
- Patients will be required to switch to Wegovy, even if Zepbound is working
- You have the right to appeal this switch, and federal law requires a decision in 72 hours
- Zepbound and Wegovy are not interchangeable – Zepbound may work better for some patients, especially those with OSA
- Claimable is building a tool to help you appeal your Zepbound denial quickly and effectively
Why is CVS Caremark suddenly denying Zepbound?
CVS Caremark, owned by CVS Health, is one of the largest pharmacy benefit managers (PBMs) in the country. They recently struck a deal with Wegovy's manufacturer, Novo Nordisk, to make Wegovy the "preferred" GLP-1 medication on its formulary. As a result, Zepbound is being dropped from coverage starting July 1, 2025, even for patients already using it with good results.
This change isn't about safety or effectiveness. It's about money. PBMs negotiate rebates with drugmakers, and these behind-the-scenes deals often determine which medication you can get – regardless of what's best for patients.

What does formulary change mean?
A formulary is the list of medications your pharmacy benefit manager (PBM) or insurer agrees to cover. When a drug, like Zepbound, is removed from the formulary, your insurance will no longer pay for it – even if it was previously approved and is working well for you.
Changes to your formulary affect your coverage – not your pharmacy. Whether you fill your prescriptions at a CVS pharmacy or elsewhere, you'll be denied coverage for Zepbound everywhere starting July 1 unless you appeal, which means it's time to understand what's changed, and make an action plan.
While Zepbound is on the out, Wegovy isn't the only GLP-1 that CVS Caremark is covering. Here's a snapshot of what CVS Caremark will and won't cover under its updated formulary:
| MEDICATION | COVERAGE STATUS |
|---|---|
| Zepbound | ❌ Not covered |
| Wegovy | ✅ Preferred drug |
| Saxenda | ✅ Covered |
| Qsymia | ✅ Covered |
| Orlistat | ✅ Covered |
| Ozempic | ✅ Covered for Type 2 Diabetes only |
| Mounjaro | ✅ Covered for Type 2 Diabetes only |
Why It Matters
Zepbound and Wegovy are not interchangeable. Zepbound uses a different mechanism of action (dual action GIP/GLP-1 receptor agonism), which means it may be more effective, and is often better tolerated – especially for people with specific conditions like obstructive sleep apnea (OSA). And older medications included on the CVS Caremark formulary – like Saxenda, Qsymia and Orlistat – are far less effective and not considered equivalent medications.
Forced switching when you've reached a stable, effective dose isn't just frustrating – it's disruptive and medically risky, potentially causing:
- Weight regain or return of symptoms
- New, intolerable, side effects
- Health setbacks and scares
- Extra clinician visits and increased costs
At Claimable, we believe your care plan should be based what's medically best for you, as determined by your doctor – not what saves your PBM money.
What to do if Zepbound is denied
If your Zepbound prescription is denied, you can file a formulary exception appeal. And in many cases, insurers are required to honor that appeal if your doctor says switching could harm you.
Here's exactly what to do.
Step 1: Get a refill before July 1
Request a 90-day refill or 30-day vacation override before July 1 (if allowed by your plan) to give you a buffer while your appeal is reviewed. This will help you avoid a care gap.
Step 2: Talk to your doctor
Reach out to your doctor now so you're ready when the July change kicks in. Ask them to:
- Be ready to file a new prior authorization for Zepbound on or after July 1.
- Write a letter of medical necessity if you decide to file your own appeal.
Step 3: File your appeal
Starting July 1, your claim for Zepbound will be denied. Once that happens:
- Submit a formulary exception request.
- This can be submitted by you or your doctor, but we recommend submitting the appeal yourself with your doctor's Letter of Medical Necessity attached. Patient appeals often have more legal rights and require responses from the insurer on faster timelines.
- This tells the insurer that Zepbound is medically necessary for you.
- Insurers must respond within 72 hours under federal law.
Less than 1% of people appeal denied claims, but those that do win about 50% of the time. You can boost your odds by following our tips below – or by using our custom tool to build the strongest possible appeal for you.
What to Include in Your Appeal
For the best chance at winning, submit an appeal letter requesting a formulary exception that explains why switching could harm you.
A strong appeal letter should include:
- Your medical results on Zepbound (weight loss, symptom control, etc.)
- Any prior medications that you've tried and failed
- Specific medical conditions like OSA that Zepbound uniquely treats
- A letter from your doctor supporting continued use
- Clinical studies, applicable laws and insurance regulations, and precedents from successful appeals with similar cases to yours
- Supporting evidence like lab results, weight logs, dosing history and medical records
Your appeal should make the case that Zepbound is working for you and that you want to avoid disruption to a stable, effective treatment plan – and be backed up by solid documentation.
Your legal rights to appeal
Under federal law, you have the right to request a medically necessary exception when a formulary change puts their care at risk.
Federal Law: 45 CFR § 156.122(c) "A health plan providing essential health benefits must have a process in place that allows an enrollee, their designee, or prescribing provider to request access to a clinically appropriate drug not otherwise covered by the plan. If granted, the plan must treat the excepted drug as an essential benefit and must respond within 72 hours." View the regulation →
On top of federal protections, many states have laws preventing insurers from forcing stable patients to switch medications mid-year. These non-medical switching or continuity of care laws may guarantee:
- You can't be forced to switch if the medication is working.
- Your doctor can override the change with a written statement.
- You must get advance notice and a clear process to stay on your current drug.
- When an exception is granted, your copay and coverage tier must stay the same.
Check here to see the non-medical switching laws enacted in your state – especially if you live in California, Illinois, Texas, or another protected state.
What to do if you get denied again
If your first appeal is rejected:
- File a second-level appeal or request an external medical review, depending on what the denial says is your next step. You have a right to multiple appeals and many people win and the second try, especially when an independent reviewer is involved.
- File a complaint with your state's Department of Insurance, especially if they refuse to give you a timely decision or fail to have a qualified clinician give you a full, fair review.
- Let your employer know—they can override the PBM if you're on a self-funded plan.
CVS has tried this before – and patients fought back
In 2022, CVS removed the life-saving blood thinner Eliquis from its formulary, forcing 150,000 patients to switch. After public outcry, provider backlash and reports of serious strokes and heart attacks, they reversed course.
We believe they can – and should – do the same here. We encourage you to consider signing the petition demanding they reverse the policy.
Create the strongest possible appeal, the easy way
From the right clinical studies to specific appeal precedents that apply to your unique circumstances, at Claimable we know how to fight – and win – forced switches like these.
Our fast, affordable tool helps you fight back. Our platform:
- Creates a personalized appeal letter backed by evidence
- Walks you through the process step by step, so you can get your appeal done in minutes, not days
- Compiles and ships your appeal not just to your insurer, but to other relevant parties like your state's Department of Insurance, HHS, and others – so your insurer knows you mean business.
Frequently Asked Questions
Does CVS Caremark cover Zepbound? No. As of July 1, 2025, Zepbound is being removed from the CVS Caremark formulary.
Can I appeal the switch to Wegovy? Yes. You have the legal right to request a formulary exception for medical necessity.
Is Wegovy the same as Zepbound? No. Zepbound uses dual GIP/GLP-1 action and may work better for some patients.
Will Medicare cover Zepbound? Aetna Medicare plans often exclude weight loss drugs like Zepbound. Appeals here may be more difficult, but not impossible.
Final Word: Your Care. Your Rights.
If Zepbound works for you, you have every right to fight for it. Forced switches driven by rebates, not results, are wrong. Claimable is here to help you fight back.
Start your appeal now to protect your care.
Annual Awards Recognize Innovative Companies and Projects Addressing the World’s Most Urgent Challenges
Recognition Follows Claimable’s Launch of GLP-1 Support, Helping Patients Navigate One of the Most Denied Treatments in the U.S.
Sacramento, CA - [June 10, 2025] - Claimable is proud to announce that it has been named to Fast Company’s 2025 World Changing Ideas Awards list. This annual recognition honors bold and transformative efforts that tackle the world’s most pressing issues—from fresh sustainability initiatives and cutting-edge AI developments to ambitious pursuits of social equity helping mold the world.
Every year, 850 million healthcare claims are denied, forcing millions of Americans to choose between medical care and financial stability. Claimable is tackling this healthcare crisis with the first AI-powered appeals platform, helping patients and providers fight back against unjust denials. Patients upload their denial notice and insurance information, answer a few questions, and Claimable does the rest, analyzing clinical research, policy details, appeals data, and their unique medical story to generate and submit a customized appeal in minutes.
This year’s awards showcase 100 outstanding projects. A panel of Fast Company editors and reporters selected the winners from a pool of more than 1,500 entries and judged applications based on their impact, sustainability, design, creativity, scalability, and ability to improve society.
“The World Changing Ideas Awards have always been about showcasing the art of the possible,” says Fast Company editor-in-chief Brendan Vaughan. “We’re proud to recognize the organizations and leaders that are making meaningful progress on the biggest issues of our time.”
Since launching in late 2024, Claimable has recovered nearly $6 million for patients, boasting an over 80% success rate across more than 70 commonly denied treatments, including autoimmune and migraine medications, IVIG for children with PANS/PANDAS, and now GLP-1s for obesity and type 2 diabetes. For the millions facing treatment delays or crushing medical debt, Claimable offers hope, making the appeals process simple, fast, and effective, getting patients the care they deserve.
“We’re using AI to solve a deeply human problem,” said Claimable Co-Founder and Chief AI Officer Zach Veigulis. “Fast Company’s recognition reinforces what we’ve always believed at Claimable, that AI can be used to make life better. At a time when technology is often used to cut costs and deny care, we’re proving it can expand access and return power to patients.”
This recognition comes as Claimable expands its impact with support for GLP-1 medication appeals. One of today's most denied treatment categories, GLP-1s like Ozempic, Mounjaro, Zepbound, and Wegovy have transformed care for people with obesity and type 2 diabetes. However, patients are often denied access due to formulary exclusions, overly restrictive eligibility criteria, or insurer mandates to “fail first” on older or less effective treatments. With over 137 million U.S. adults now eligible for GLP-1 support, Claimable offers patients and providers a purpose-built solution designed to overcome the unique challenges of GLP-1 coverage denials.
"Insurance denials aren't just a paperwork issue, they're a public health crisis hiding in plain sight," said Alicia Graham, co-founder and COO at Claimable. "While others patch old systems, we're building something entirely new. We're reimagining how healthcare access should work, using technology to turn the tables on a system that's stacked against patients. That's why we've built Claimable alongside the people most affected: patients and providers. Our platform works because it doesn’t just make appeals faster, it makes them smarter, giving people the best chance to win."
Claimable is available nationwide and accepts denials from all insurance providers, including Medicare, Medicaid, United Healthcare, Anthem, Aetna, Cigna, and BCBS plans. To learn more about Claimable and all the treatments they support, visit www.getclaimable.com.
###
ABOUT CLAIMABLE
Claimable revolutionizes the way patients and providers fight healthcare denials, helping ensure everyone has access to the care they need and the coverage they deserve. The platform leverages purpose-built AI to analyze clinical research, policy details, appeals data, and patients’ unique medical stories, generating and submitting customized appeals in minutes. Claimable is available nationwide, accepting denials from all insurance providers, including Medicare and Medicaid. A NVIDIA Inception Program member, Claimable continues to push the boundaries of AI innovation in healthcare. For more information: www.getclaimable.com.
Contact:
Emily Fox

At Claimable, we believe healthcare should reflect the best of what we know—not be constrained by inertia, stigma, or financial incentives that prioritize profit over patient care.
Right now, that belief is being tested. Patients eligible for GLP-1 medications are being denied coverage—denials often based on arbitrary criteria that ignore clinical guidelines and FDA approvals. As the science accelerates, coverage is moving in the opposite direction—not because the evidence has changed, but because the rebate math doesn’t work for payers.
That’s why we’re expanding our platform to support appeals for GLP-1s. We already know that the conditions they treat are urgent—affecting over half of US adults and driving a disproportionate share of preventable healthcare costs—and with compounded versions of these medications unavailable as of May 22nd, the need is more pressing than ever.
What the science is telling us
GLP-1s have evolved far beyond their original use for type 2 diabetes and weight loss. Today, they are FDA-approved not only for managing blood sugar and reducing body weight, but also for treating obstructive sleep apnea and lowering the risk of serious cardiovascular events like heart attacks and strokes.
In advanced stages of clinical review, GLP-1s are also showing promise for treating metabolic dysfunction-associated steatotic liver disease (MASLD), chronic kidney disease (CKD), pre-diabetes, diabetic retinopathy and osteoarthritis of the knee (in patients with obesity).
And the emerging science is even more far-reaching. Early research suggests that GLP-1s may play a role in reducing neuroinflammation associated with Alzheimer’s, Parkinson’s and dementia; curbing addictive behaviors tied to substance use; improving symptoms of irritable bowel syndrome (IBS), and even impacting certain types of cancer. The list of ways these medications can change — and save — lives is profound and growing fast.
For many of us, this isn’t just promising science. It’s deeply personal.
One area that strikes particularly close to home for me is metabolic dysfunction-associated steatotic liver disease (MASLD) —a condition that affects nearly a third of U.S. adults and has no approved treatment. I lost my father to complications of diabetes, including MASLD. By the time he was diagnosed, he was already suffering from liver failure. A catastrophic upper gastrointestinal bleed and emergency medical evacuation followed. It was marked by a single week that aged me years.
If therapies like this had been available earlier—maybe it would have changed the outcome.
These medications don’t just improve quality of life — they help prevent the cascade of complications that make care more expensive, less effective, and harder to access. A recent analysis of over 50 million insured lives found that GLP-1 users experienced 44% fewer hospitalizations for major cardiovascular events, and healthcare spending rose at just half the rate of similar non-users by year two.
When people stay healthier longer, it means fewer emergency interventions, fewer disability claims, and more stable, productive lives.
As new treatments emerge, access to GLP-1s is slipping away.
GLP-1s are no longer just a type 2 diabetes or weight loss drug. They represent a platform therapy with far-reaching potential across some of the most costly, intractable diseases in healthcare—and yet, access is moving in the wrong direction.
Statins. Insulin analogs. SGLT2 inhibitors. Each faced early resistance. Each is now a pillar of care. GLP-1s are on the same trajectory—but patients can’t afford to wait years for coverage to catch up.
The barriers to coverage aren’t scientific. They’re systemic. And these delays and denials don’t just hurt patients. They affect providers, employers, and the healthcare system as a whole.
With compounded versions of branded GLP-1s off the market as of May 22, 2025, affordability has collapsed. Direct-pay options run $400 to $700 a month—pricing out the majority who should qualify for initial or continued treatment. Copay cards and assistance programs offer temporary relief—but they’re not available to everyone, and they don’t solve the broader access problem.
Those who attempt to gain coverage face increasingly restrictive and often arbitrary criteria. From BMI requirements that far exceed standard criteria, to mandating costly weight management programs and shrinking approval windows from 12 months to just one, new barriers are being constantly invented and implemented to limit access.
Turning evidence into access—one appeal at a time.
At Claimable, we help patients push back. We handle the administrative burden—challenging denials, navigating appeals, and ensuring every request is grounded in current science, regulatory precedent, and standard of care.
GLP-1s are the next frontier in chronic disease prevention. But for patients to benefit, access must match the evidence.
The dream is to prevent people from becoming patients, to keep them present in their lives.
We’re here to make that happen— appeal by appeal. We’re ready to go.
Warris Bokhari
CEO, Claimable
Featured stories
In the news
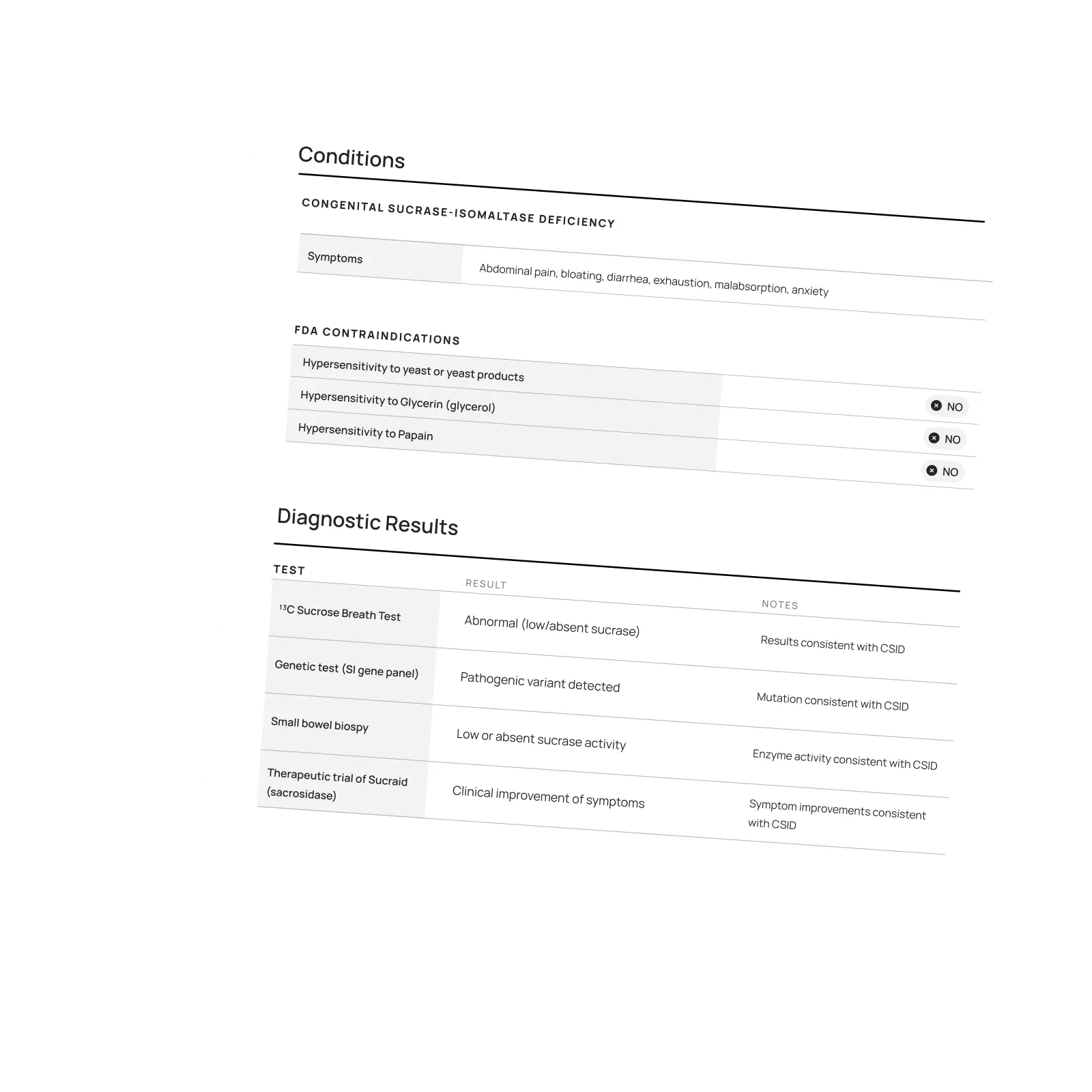
Download a winning sample appeal
Want to see what it takes to successfully overturn a health insurance denial? Download our sample appeal to learn how we build strong, evidence-based cases that get results.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Each month, I endure about eight major episodes, each one leaving me exhausted, unable to concentrate, and too unwell to take part in daily life.
The frequency and unpredictability of these symptoms have isolated me socially and limited my capacity to take part in activities most people take for granted.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!

One of our core principles is to help patients protect their rights and level the playing field with their insurance company. This includes rights to multiple appeals, fair reviews, decision rationale, exceptions when needed, and adequate network access, among others. For more, read our post on patients rights.
Claimable’s AI-powered platform analyzes millions of data points from clinical research, appeal precedents, policy details, and your personal medical story to generate a customized appeals in minutes. This personalized approach sets Claimable apart, combining proprietary and public data, advanced analysis and your unique circumstances to deliver fast, affordable, and successful results.
We currently support appeals for over 85 life-changing treatments. Denial reasons may vary from medical necessity to out of network, and we even cover special situation like appealing plans that won’t count your copay assistance towards your deductible (hint: those policies were banned at the federal level in 2023). That said, we are rapidly growing our list of supported conditions, treatments and reasons. You can quickly check eligibility and ask to be notified when your interest becomes available. It helps us know where to focus next 🙂
We think about appeal times in a few ways. First, many professional advocates and experienced patients spend 15, 30 or even 100 hours building an appeal–but with Claimable, this takes minutes. We automate the process of analyzing, researching, strategizing and wordsmithing appeals. Next, there is the process of figuring out where you will send it (hint: expand your reach beyond appeal departments), then printing, mailing and/or faxing your submission. We handle that, too. Finally, there is the time it takes to get a decision. We request urgent reviews when appropriate, and typically receive standard appeal decisions within a couple weeks.
Review periods are mandated by applicable laws, from 72 hours for urgent, 7 days for experimental, 30 days for upcoming and 60 days for received services. Our goal is to get a response as fast as possible, since most of our clients are experiencing long care delays or extreme pain and suffering.
Claims are denied for a variety of reasons, many of which blur definitions. We focus on helping people challenge denials by proving care is needed and meets clinical standards, in addition to addressing specific issues like experimental treatments, network adequacy, formulary or site of care preference exceptions. We don't support denials for administrative errors or missing information, as we think those are best handled by simply resubmitting the claim in partnership with your provider. That said, many of our most rewarding successes have been cases previously though 'unwinnable', with providers and patients who fought tirelessly for months without appropriate response or resolution.
A denial letter is a formal notice from your insurance company explaining why a claim was denied and how you can appeal the decision. Sometimes the notice is included within an Explanation of Benefits. It is a legal requirements; if you didn’t receive one, contact your insurance company.
A letter of medical necessity is a statement from your doctor justifying why a specific treatment is critical to your care and/or urgently needed. You can attach it to your patient appeal to strengthen your case, especially if you are requesting an urgent appeal or need to skip standard ‘step therapy’ requirements. That said, we don’t require them and are often successful without them.
A claim file contains all the documents and communications your health plan used to decide whether to approve or deny your claim. Most health plans are legally required to share this information upon request. According to a ProPublica investigation, reviewing your claim file can help expose mistakes or misconduct by your health plan, which can make your appeal stronger.
Your insurer is required by law to give you written information about how to appeal, including the name of the company that reviewed your claim and where to send your appeal. Your health insurer may work with other companies, such as Pharmacy Benefit Managers (PBMs), Third-Party Administrators (TPAs), or Specialty Pharmacies, to manage your claims. These companies might be responsible for denying your claim and handling the appeal process on behalf of your insurer.
If you don't win your first appeal– don't give up! Many people are successful on their 2nd, 3rd or even 4th try, and future appeals are reviewed by independent entities. That said, we wrote a whole guide to understanding your options, including escalating your appeal and seeking other assistance for covering costs, forgiving debt or even seeking legal or regulatory support.
While both denial rates and appeal success rates vary widely by the type of health plan, state, and insurance company, studies have shown more than 50% of people win their appeal–and we apply strategies to boost your chances of success. Claimable has an 80% appeal success rate. The biggest denial challenge is that most people never appeal–allowing unjust denials to control their healthcare options because they are unaware of their rights or lack the support needed to fight back. No one needs to fight alone–Claimable is here to help. We know first hand that many denials are based on errors, inconsistencies or auto-decisions, and have proven strategies for fighting back against this injustice.
Let’s get you covered.