FEP Blue formulary changes 2026: How to keep coverage for Dupixent, Zepbound, and more

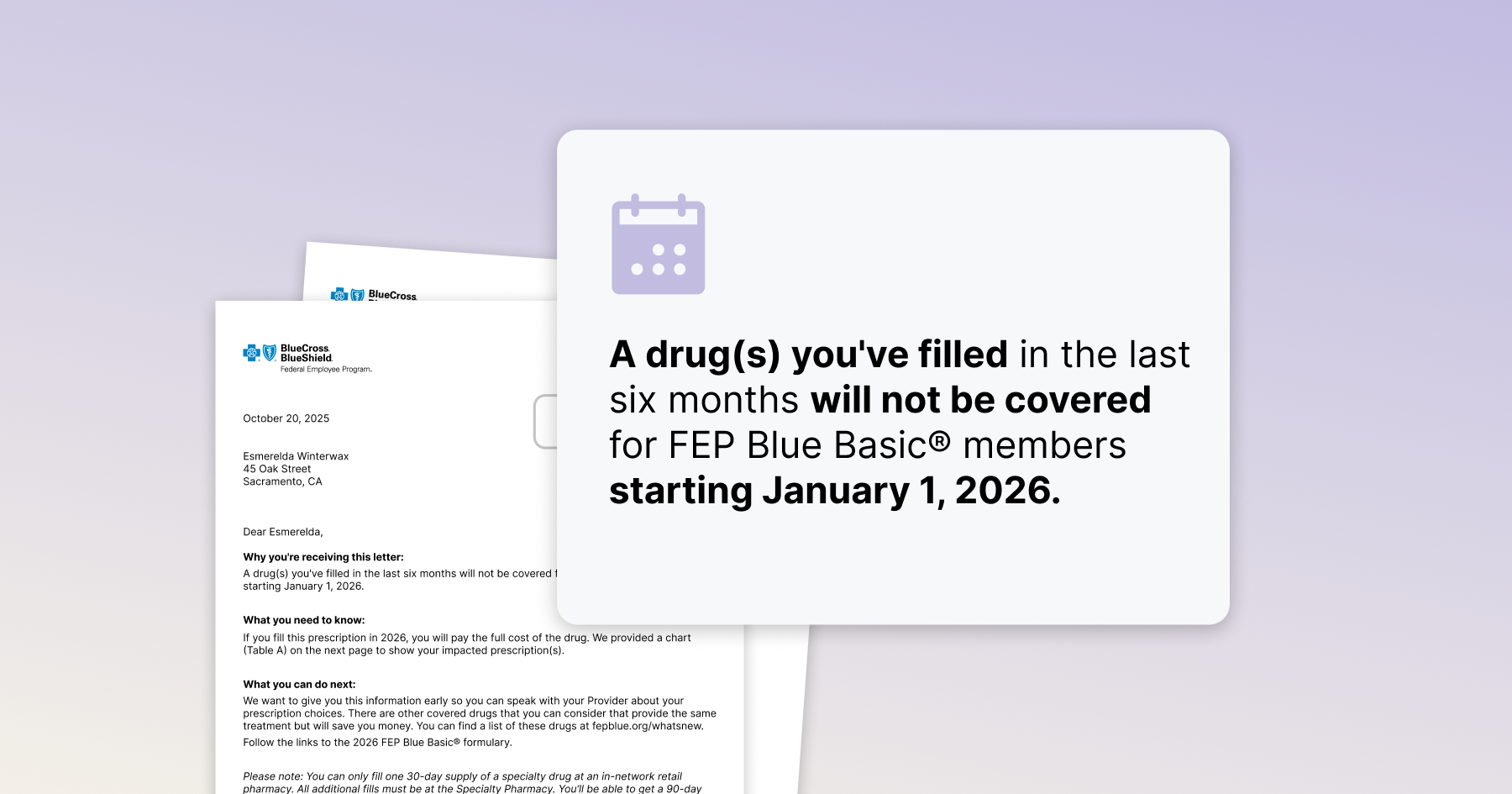
Got a letter about 2026 coverage changes? You’re not alone. BCBS Federal Employee Plans (FEP Blue) are dropping Dupixent, Zepbound and many more from its list of covered drugs.
That means that thousands of people are being told that a medication they’re taking won’t be covered next year – and wondering what to do now.
Let’s cut to the chase: You have options. You don’t have to switch to another drug or pay out of pocket. When formulary changes happen, you can fight back. You do this by requesting a “formulary exception” that lets you stay covered.
Here’s what’s going on, and what you can do about it.
Quick summary
- What changed: Dupixent, Zepbound and more are listed as not covered in 2026 on some FEP Blue options.
- You can fight the change: File an appeal for a formulary exception. If you win, they have to cover your treatment.
- What to do now: Start your appeal now – so you don’t have a gap in January.
- More questions? Check out our resources below.
- For Dupixent -> FEP Blue formulary exception request guide
- For Zepbound -> Formulary switch appeals
What changed — and why it matters
This is a formulary change. PBMs and plans update drug lists annually and decide to “prefer” alternatives based on their contracts with the manufacturer.
In this case, they are removing Zepbound, Dupixent, and others, and pointing you to other options.
The full list of formulary changes for 2025:
It’s important to know that those preferred alternatives, however, aren’t always equivalent – they may be less effective, not appropriate for your specific history, or have other considerations involved. If you’re stable on Dupixent or Zepbound, you shouldn’t have to switch just because insurance says so.
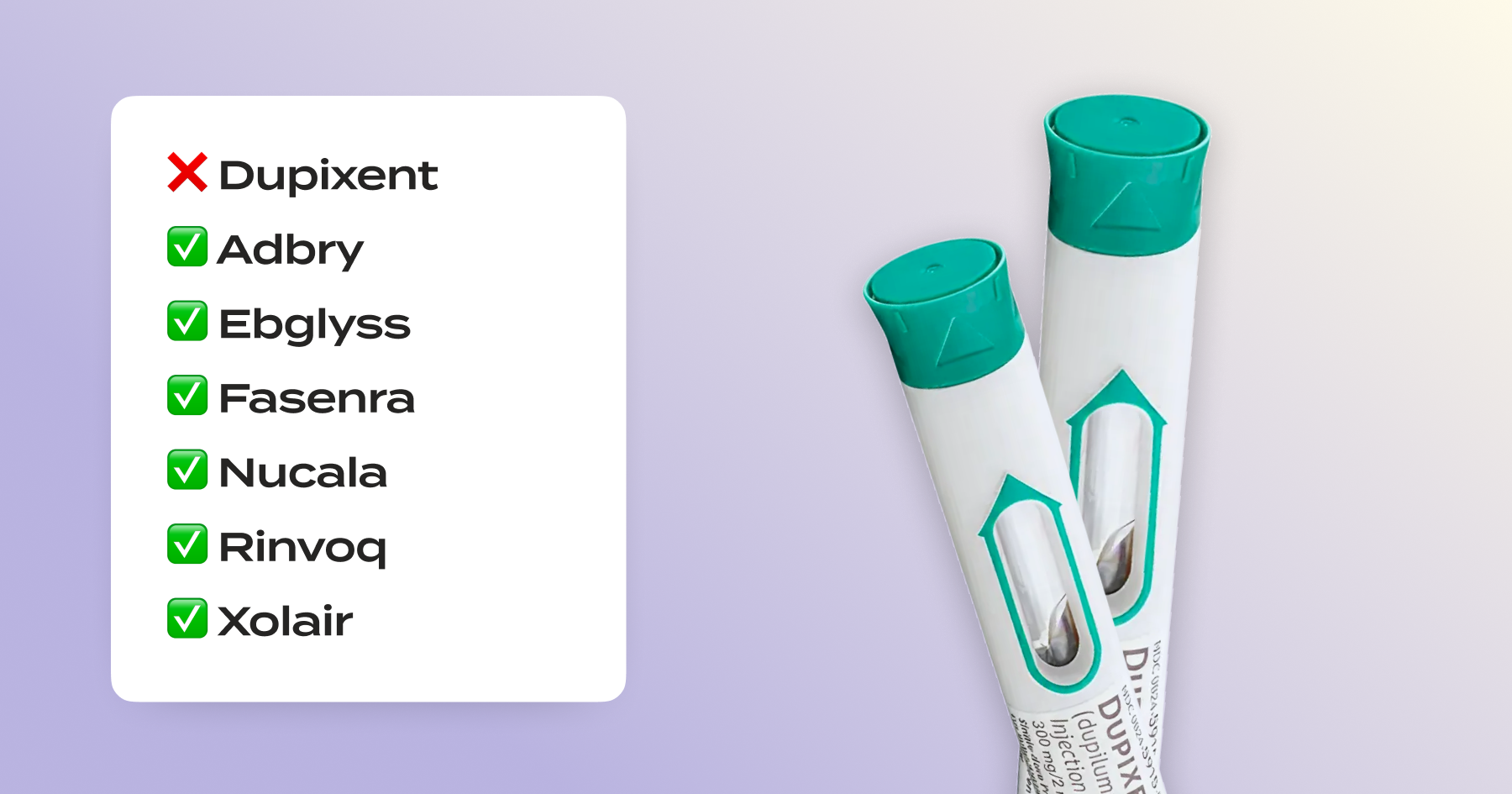
What’s covered on the FEP Blue formulary instead
Both Zepbound and Dupixent are approved to treat multiple conditions. So even though your plan might say, for example, that Fasenra is an alternative option for Dupixent, it doesn’t mean that Fasenra is applicable or FDA-approved for your specific condition.
Check out our breakdown below to see the alternatives and what conditions they’re indicated for.
Dupixent - covered alternatives by FDA-approved indication
Zepbound - covered alternatives by FDA-approved indication
Requesting a formulary exception as an FEP Blue member
You have a legal right to request that they make an exception and cover your medication. Here’s how it works:
- You or your doctor can submit the request. It’s nice when your doctor is willing to request on your behalf, but doing it yourself has benefits: including more powerful legal rights and the ability to escalate to a second review, giving you a better chance to win. Using Claimable makes it easy to do your own appeal.
- Tip: Provider appeals and patient appeals are two different “paths” to request a formulary exception. You can do them both simultaneously if you want to.
- You can appeal now, ahead of 2026. If you got the notice that you won’t be covered, you can use it to start fighting for coverage. We recommend starting now – because you can still appeal again if you get denied in 2026.
- Putting together your request. Write a letter making the request. Include your diagnosis, your response to the medication, what you’ve tried in the past and why the alternatives won’t work for you. You can follow our DIY guide, or use Claimable to create your appeal and fax and mail it for you.
- Get it in the mail (yes, snail mail). If you’re doing it yourself, mail your appeal to Service Benefit Plan, P.O. Box 52080, Phoenix, AZ 85072-2080 or fax to 1-877-378-4727. If you use Claimable, we do that for you.
- If you get denied, don’t give up. If FEP upholds the denial you can escalate your appeal by requesting a second administrative review by the Office of Personnel Management.
Read our Dupixent DIY appeal guide here – or use Claimable to create and send your appeal today.
FAQs
Will FEP Blue cover Dupixent in 2026?
Not without a formulary exception. The preferred drugs are Adbry, Ebglyss, Xolair, Nucala, Fasenra, and Rinvoq.
The good news is that insurers can’t make you switch for non-medical reasons if you’re doing well on your current treatment. 33 states even have laws that prevent switches like these.
While we can’t guarantee that you’ll win, a strong appeal like the ones we write at Claimable – making an expert-backed clinical, legal, and policy argument for coverage – gives you the best chance.
Will FEP Blue cover Zepbound in 2026?
Not without a formulary exception. The preferred drugs are Wegovy, Saxenda, Contrave, Qsymia, and Xenical.
The good news is that insurers can’t make you switch for non-medical reasons if you’re doing well on your current treatment. 33 states even have laws that prevent switches like these.
While we can’t guarantee that you’ll win, a strong appeal like the ones we write at Claimable – making an expert-backed clinical, legal, and policy argument for coverage – gives you the best chance.
What are my chances of winning my formulary exception request?
The majority of people who submit an appeal win. At Claimable, we’re experts at fighting formulary changes like this one – and we take them all the way to the top if we have to.
Is there a FEP Blue “formulary exception form” for members?
The form in your letter is usually for prescribers. Members file a reconsideration/appeal directly. Follow the steps above to file yours.
Where do I mail my FEP appeal?
Mail your appeal to Service Benefit Plan, P.O. Box 52080, Phoenix, AZ 85072-2080 or fax to 1-877-378-4727. Or use Claimable to do it for you.
What phone number can I call for pharmacy questions?
FEP Pharmacy: 877-378-4727. (For appeals, mail/fax to the address on your EOB.)
How do I write a Dupixent appeal letter?
Briefly state the request, your diagnosis, prior therapies and outcomes, current response, and why listed alternatives are not appropriate. Or use Claimable to automatically create a strong letter in minutes! For eligible Dupixent patients, it’s completely free.
How much does Claimable cost?
For Dupixent, appeals for FEP Blue denials are completely free thanks to our partnership with Dupixent’s patient support program. For Zepbound, appeals are $39.95+shipping. Affordability is important to us at Claimable – please reach out to our support team if you have any questions about your appeal and our costs.
What medications does Claimable support?
Claimable supports over 85 commonly denied medications. Of the drugs excluded from the 2026 FEP formulary, we support appeals for Dupixent, Cinqair, Tezspire, Zepbound, Enbrel, Hyrimoz, Otezla, Rinvoq, Skirizi, Taltz, Tremfya, and Xeljanz.
What are all of the formulary changes for FEP plans?
FEP Blue Basic and Standard are dropping coverage for a variety of medications in 2026 – not just Dupixent and Zepbound. Here are the top drugs that were covered in 2025 that are not covered in 2026. Find your formulary here for the full list + details on what’s covered, indications, and more.
- Biologics & immunology: Cibinqo, Cinqair, Dupixent, Nemluvio, Tezspire, Enbrel, Hyrimoz, Otezla, Pyzchiva, Rinvoq, Skyrizi, Taltz, Tremfya, Tyenne, Xeljanz, Yesintek
- Multiple sclerosis: Aubagio (brand), Bafiertam, Gilenya (brand), Mavenclad, Ponvory, Tecfidera (brand), Vumerity
- Dermatology & acne: benzoyl peroxide (6% cloth, 8% gel, 5% wash), Benzac AC Wash 5%, some variants of Benzepro, Differin (Rx version), PR Benzoyl Liq 7%, Zaclir, Sofdra
- Weight loss / obesity: Zepbound
- Cancer: Imkeldi, Phyrago, Danziten, Sutent (brand; generic sunitinib preferred), Gilotrif
- ADHD: amphetamine (generic for Evekeo), amphetamine ER ODT, dextroamphetamine solution, methamphetamine (generic for Desoxyn), Procentra, Onyda XR
- Neurological & psychiatric: Igalmi, Raldesy, chlordiazepoxide/amitriptyline, Forfivo XL, Erzofri, Bucapsol, Pamelor, Opipza
- Headache & tension: Allzital, Fioricet
- Growth hormone: Ngenla, Skytrofa, Sogroya
- Testosterone: Kyzatrex, Tlando, Undecatrex
- Thyroid: Ermeza, Thyquidity
- Cardiovascular & hypertension: Accupril, Lotensin HCT, Lotrel, Prestalia, Aspruzyo Sprinkle, Catapres-TTS (generic clonidine patch preferred)
- Hematology & sickle cell: Alvaiz, Droxia
- Metabolic & rare endocrine: Javygtor, Zelvysia, Livdelzi, Iqirvo
- Gastrointestinal & Hepatobiliary: Mytesi, Omeclamox, Chenodal, Urso Forte (generic ursodiol preferred)
- Rare & Orphan: Sohonos, Xuriden, Zokinvy
Helpful links
- FEP Blue 2026 Formulary Guide
Step by step guide to a formulary exception - Zepbound formulary changes - what to do if you don’t want to switch to Wegovy
- Your rights if FEP Blue denies coverage (appeals, urgent review, OPM)
Final word
When your insurer changes their formulary, it’s almost like they’re saying “just switch to this other medication, it’s easy!”. But they don’t know your history, past treatments, and specific details. If Dupixent or Zepbound is the right fit, they can’t just make you switch.
Before you switch, appeal. So you can stay on what works for you.
Get started today.
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!